The artificial pancreas (AP), known as closed-loop control of blood glucose in diabetes, is a system combining a glucose sensor, a control algorithm, and an insulin infusion device. AP developments can be traced back 50 years to when the possibility for external blood glucose regulation was established by studies in individuals with type 1 diabetes using intravenous glucose measurement and infusion of insulin and glucose. After the pioneering work by Kadish (1) in 1964, expectations for effectively closing the loop were inspired by the nearly simultaneous work of five teams reporting closed-loop control results between 1974 and 1978: Albisser et al. (2), Pfeiffer et al. (3), Mirouze et al. (4), Kraegen et al. (5), and Shichiri et al. (6). In 1977, one of these realizations (3) resulted in the first commercial device—the Biostator (7; Fig. 1), followed by another inpatient system, the Nikkiso STG-22 Blood Glucose Controller, now in use in Japan (8).
FIG. 1.
The Biostator (courtesy of William Clarke, University of Virginia).
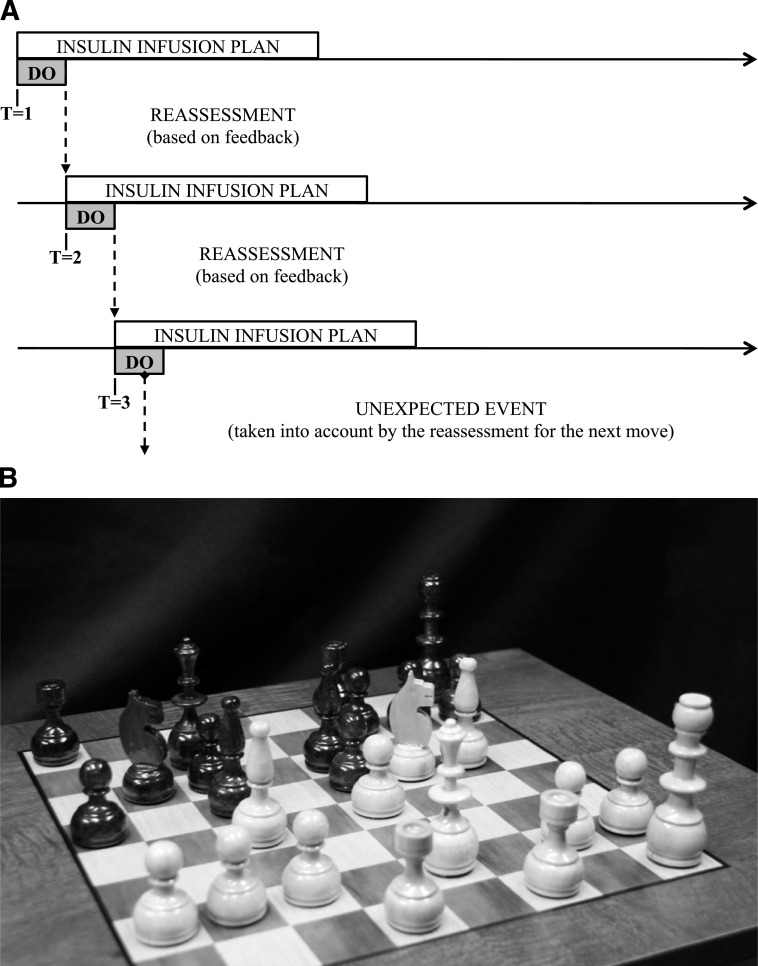
Although the intravenous route of glucose sensing and insulin infusion is unsuitable for outpatient use, these devices proved the feasibility of external glucose control and stimulated further technology development. Figure 2 presents key milestones in the timeline of AP progress.
FIG. 2.
Key milestones in the timeline of AP progress. EU, Europe; IP, intraperitoneal; NIH, National Institutes of Health; SC, subcutaneous.
In 1979, landmark studies by Pickup et al. (9) and Tamborlane et al. (10) showed that the subcutaneous route was feasible for continuous insulin delivery. Three years later, Shichiri et al. (11) tested a prototype of a wearable AP, which was further developed in subsequent studies (12,13). In the late 1980s, an implantable system was introduced using intravenous glucose sensing and intraperitoneal insulin infusion (14). This technology was further developed, leading to clinical trials and long-term use (15,16); however, its clinical application remained limited because of the extensive surgical procedures needed for sensor and pump implantation.
In all early intravenous and intraperitoneal AP systems, the closed-loop control algorithms belonged to a class known as proportional-derivative controllers, which used blood glucose values and blood glucose rate of change in a relatively straightforward calculation of insulin dose. However, as it is explained later in this article, proportional-derivative control and its enhanced version, proportional-integral-derivative control, have inherent limitations that hinder their use in subcutaneous systems because of unavoidable time lags in subcutaneous glucose sensing and insulin action. Newer controllers, known as model-predictive control (MPC), avoid these limitations by using a mathematical model of the metabolic system of the person being controlled in their calculations. Many of these MPC algorithms are based on another 1979 milestone, the Minimal Model of Glucose Kinetics (17). Thus, since the early years of AP development, glucose sensing and insulin delivery technologies were accompanied by computer modeling and simulation (18–22). Review of methods for glucose control prior to 2000 can be found in two concurrent papers (23,24).
The new wave—subcutaneous AP—developed after minimally invasive subcutaneous glucose sensing was commercially introduced in 1999 by the MiniMed continuous glucose monitoring (CGM) system. This set off an accelerating academic and industrial effort focused on the development of a subcutaneous-subcutaneous system (Fig. 2). The MiniMed (later, Medtronic) closed-loop project was the first to provide evidence for the feasibility of the subcutaneous-subcutaneous route for fully automated blood glucose control in type 1 diabetic patients (25). The 3-year ADICOL project funded by the European Commission showed the feasibility of using advanced MPC strategies to close the loop (26). In September 2006, the Juvenile Diabetes Research Foundation International (JDRF) initiated the Artificial Pancreas Project and funded a consortium of centers to carry out closed-loop control research. So far, encouraging results have been reported by several centers (27–31). Two notable achievements were the acceptance by the Food and Drug Administration of the University of Virginia–University of Padova type 1 diabetes simulator as a substitute to animal trials in the preclinical testing of closed-loop control strategies (32), and the design by a team from the University of California Santa Barbara and the Sansum Diabetes Research Institute of a communication platform allowing the automated transfer of data between CGM, control algorithm, and insulin pump (33). Following these developments, JDRF initiated a now-ongoing multicenter, multinational trial in adults and adolescents with type 1 diabetes. Additional momentum was brought by the U.S. National Institutes of Health (NIH) funding several AP projects in 2009 and by the European Commission launching the AP@Home project in 2010, which involves seven universities and five companies throughout Europe. In the wake of these rapid developments, this article aims to identify critical problems in AP development and to outline possible solutions and a pathway toward the clinical acceptance of ambulatory closed-loop control.
Limitations of current glucose sensors
CGM technology was introduced 10 years ago, initially as a method for retrospective review of glucose profiles (34–36). Shortly after, real-time devices came about, providing online glucose readings (37). These first devices had limited performance, particularly in the hypoglycemic range (36,38,39). Since then, significant progress has been made toward versatile and reliable CGM; a number of studies have documented its benefits (40–42) and charted guidelines for its clinical use (43,44). Because CGM data are the input to the AP control algorithm, understanding of the physical, biochemical, and mathematical principles and limitations of this technology is critical (45,46).
First, most of the commercial subcutaneous CGM devices measure glucose concentration in a different than blood compartment—the interstitium. However, during rapidly changing conditions, e.g., after a meal or during a hypoglycemic episode, interstitial glucose and blood glucose can be markedly different (47–49). Thus, CGM devices require calibration using one or more daily blood glucose samples. The influence on CGM accuracy of the number and timing of calibration points was assessed by several studies (50,51). In particular, the DirecNet Study Group (52) analyzed changes in accuracy by modifying the calibration retrospectively and showed that calibrating during periods of relative glucose stability significantly improves CGM accuracy. Modern calibration procedures were suggested, based on mathematical models of interstitial glucose kinetics (53,54).
Second, time lag exists because of blood-to-interstitial glucose transport and the sensor processing time (instrument delay). Because such a time lag could greatly influence the accuracy of CGM (55,56), a number of studies were dedicated to its investigation (57–61). In most studies CGM readings lagged blood glucose (most of the time) by 4–10 min, regardless of the direction of blood glucose change, but the formulation of the push-pull phenomenon brought arguments for a more complex relationship than a constant time lag (60). For the purpose of closed-loop control, mitigation of the time lag was suggested based on near-term glucose forecast methods (51,61).
Third, errors from transient loss of sensitivity, and random noise confound CGM data (62–64). Thus, filtering, denoising, and artifact rejection in CGM data are important for closed-loop control. Algorithms performing these tasks are available in commercial CGM devices (65–67). The precise tuning of filter parameters in an automatic manner is, however, a difficult problem. Advanced methods that can be used to resolve this challenge have been recently reported (50,53,68–70).
Despite of their inherent limitations, CGM devices produce rich frequently-sampled data sets (e.g., every 5–10 min) allowing them to serve as AP-enabling technology (43,45). First steps from simple monitoring to control have already been taken; modern CGM devices display trends and blood glucose rate of change and are capable of alerting the patient about upcoming hypo- or hyperglycemia (71–73). Studies of the utility of such alerts have been initiated (73–75), and the next logical step—prevention of hypoglycemia via shutoff of the insulin pump—has been taken (76).
Limitations of insulin delivery
Because of its pharmacokinetic and pharmacodynamic advantages, the intravenous route of insulin delivery has been tested for ambulatory use with implantable devices from the 1970s to the early 1990s (77,78). However, despite their effectiveness, the limitations caused by recurrent catheter complications due to blood clotting stopped the development of this route of insulin delivery (79). An alternative approach to staying close to physiology is to use intraperitoneal insulin delivery, e.g., insulin infusion via the portal venous system (80–83). In view of closed-loop glucose control, the intraperitoneal infusion route has several intriguing characteristics: reproducibility of insulin absorption combined with quick time to peak and return to baseline, close-to-physiological peripheral plasma insulin levels, and restoration of glucagon response to hypoglycemia and exercise (84–86). Although the experience of implantable programmable insulin pumps from the 1990s has highlighted their benefits including sustained improvement in mean blood glucose and reductions in glucose variability and severe hypoglycemia (87–90), the clinical use of these devices has been limited because of insulin aggregation issues (91), increased production of anti-insulin antibodies, which impair insulin action in some patients (92,93), and the cost associated with this technology. Still, the development of less invasive and cheaper implantable ports for intraperitoneal insulin delivery (e.g., DiaPort; Roche Diagnostics, Mannheim, Germany) may extend this option of insulin infusion in view of an AP (94).
Since the late 1990s, continuous subcutaneous insulin infusion (CSII) has become an accepted mode of insulin pump therapy (95). Improvements in safety, miniaturization, refined tuning of insulin pumps allowing for fine adjustments of basal rate, the recently introduced “patch pumps” (96), and new insulin analogs (97,98), all lead to improved patient comfort and better glucose control. The key issue of subcutaneous insulin delivery remains the delay in action caused by the time needed for subcutaneous absorption, resulting in late insulin peaks up to 120 min after the injection of a subcutaneous bolus of regular insulin (95). Moreover, with subcutaneous insulin delivery the lost physiological role of the liver in modulating peripheral insulin levels results in higher peripheral insulinemia (82). Whether such a reduced hepatic insulinization impairs the control of hepatic glucose output significantly is still unclear. In terms of safety, altered absorption at the subcutaneous delivery site has been pointed out as a risk for insulin underdelivery—a major issue observed with CSII, which may result in ketoacidosis if undetected and not corrected in time (77,99). This phenomenon has been shown to occur even more rapidly with the use of fast-acting analogs (100).
In an AP setting, CSII combined with subcutaneous glucose sensing has been shown to be effective for “out-of-meal” periods, keeping blood glucose in the normal range in the postabsorptive state (26,45). However, fully automated closed-loop control has not been so successful in addressing insulin needs at meals (25,26). Indeed, the rapid rise of postmeal glucose is difficult to avert because of the inherent delays in subcutaneous insulin absorption and action (101). As a result, all AP trials reported to date show a significant postprandial glucose peak above the normal range. Moreover, delayed insulin action while postprandial blood glucose decreases may result in secondary glucose lows a few hours after the meal (26).
Need for “smart” control algorithms
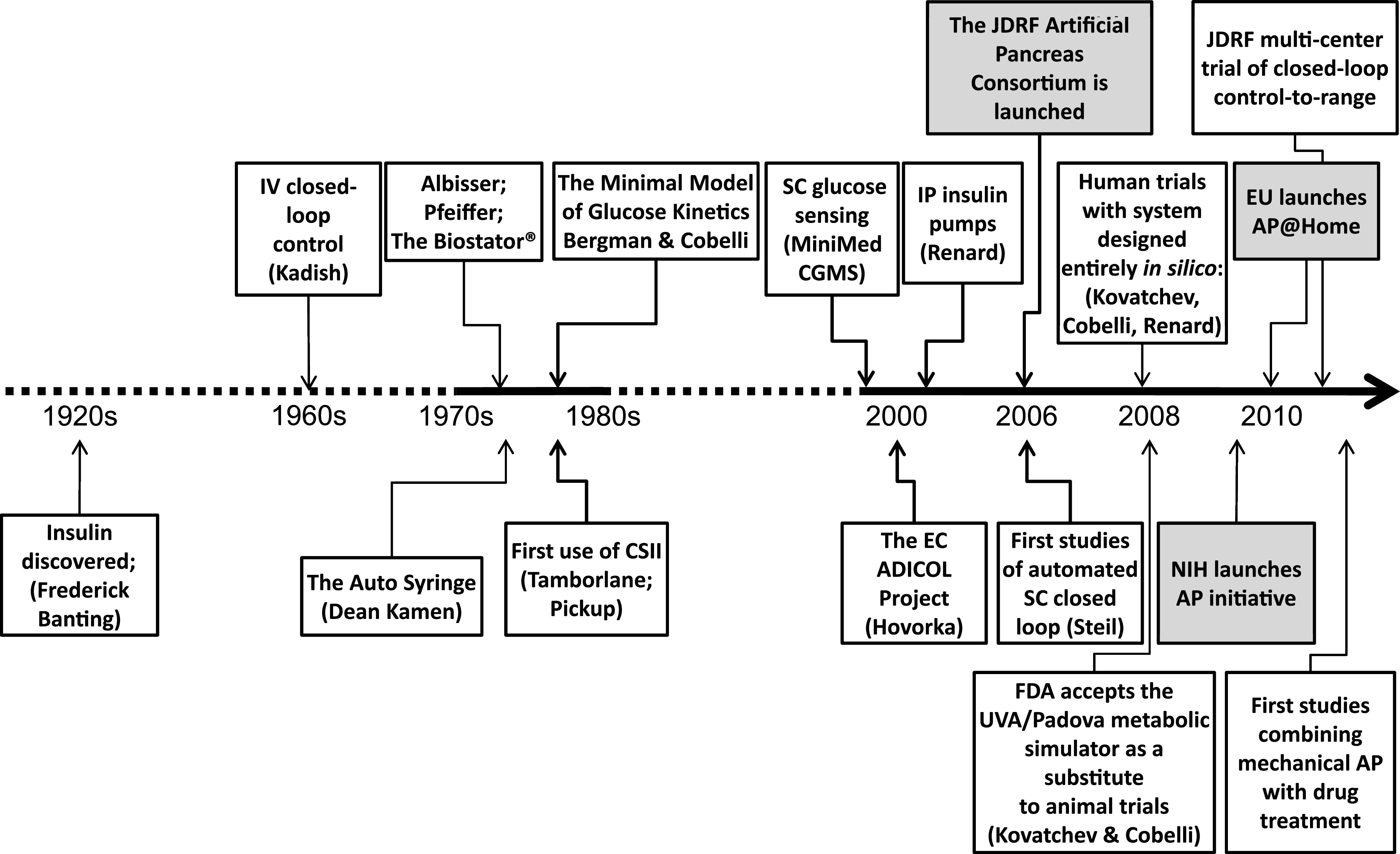
Despite important developments in sensor and pump technology, the AP must cope with the delays and inaccuracies in both glucose sensing and insulin delivery described in the previous sections. This is particularly difficult when a system disturbance, e.g., a meal, occurs and triggers a rapid glucose rise that is substantially faster than the time needed for insulin absorption and action (Fig. 3).
FIG. 3.
Block diagram of closed-loop glucose control. Three major delays are indicated: insulin absorption (regular and ultrafast insulin), insulin action on peripheral tissues and on the liver, and sensing in the interstitium.
The problem is that with inherent delays, any attempt to speed up the responsiveness of the closed loop may result in unstable system behavior and system oscillation. Thus, a sound controller design must consider a relatively slow response, giving time for the delays to wear off before the next control action. However, a slow response cannot provide good attenuation of postprandial glucose peaks. Hence the principal AP control dilemma: find a trade-off between slow-pace regulation well suited to mild control actions applicable to quasi-steady state (e.g., overnight), and postprandial regulation calling for prompt and energetic corrections (102,103).
Historically, this problem was clearly demonstrated by the first closed-loop experiments that used PID algorithms. Because PID is purely reactive, responding to changes in glucose concentration after they have occurred, it suffers most from the problems described above. In particular, to avoid hypoglycemia after a meal, one has to design a moderately aggressive controller; however, such a “cautious” design would not react promptly and effectively to meals. To improve PID performance, one possibility is to add a feed-forward action (a regular premeal bolus), which helps with meal compensation as demonstrated in clinical studies (27). To mitigate hypoglycemic events, an insulin negative feedback on insulin delivery rate has also been introduced (104).
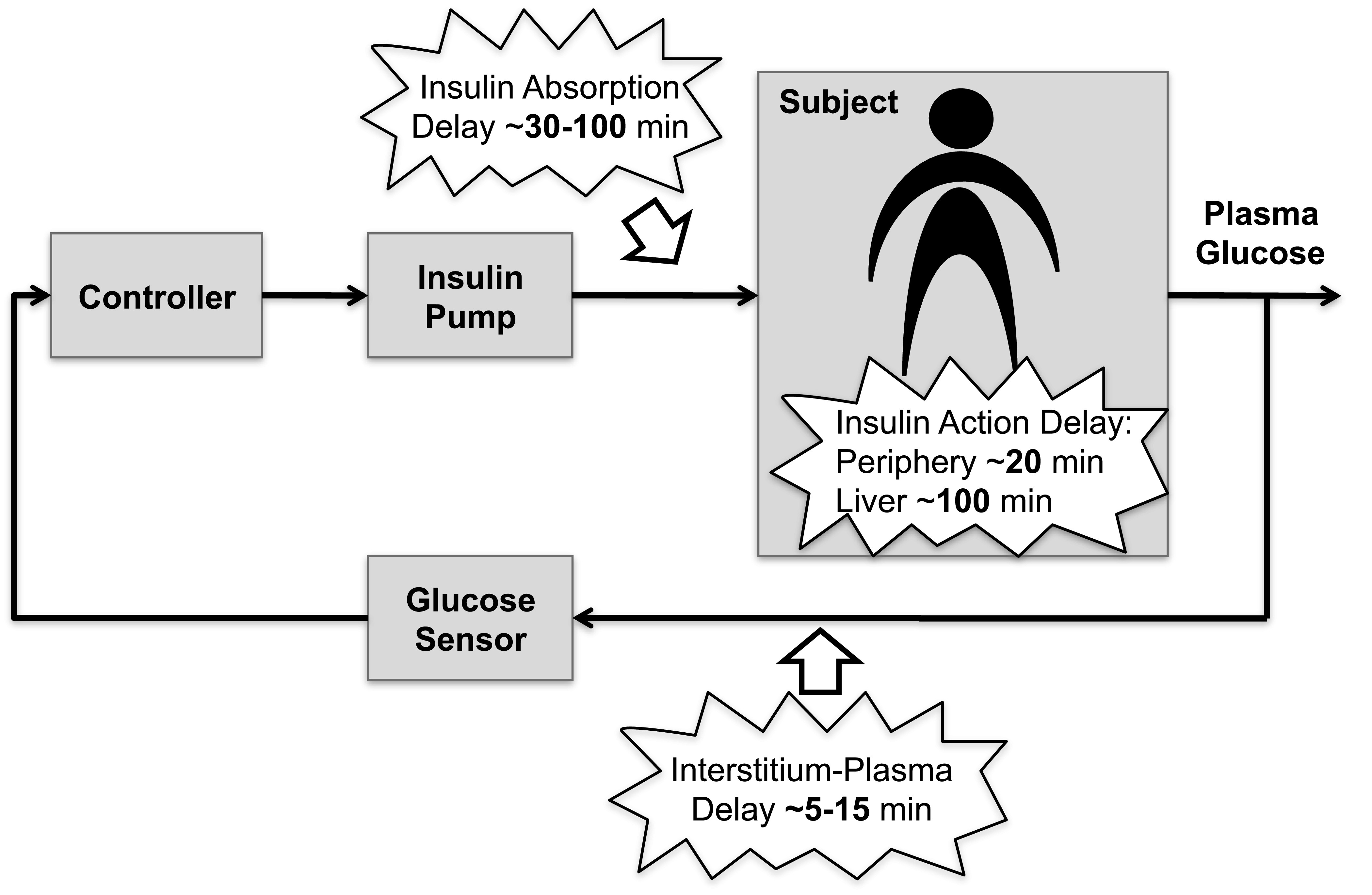
The new wave of control designs, MPC, is based on prediction of glucose dynamics using a model of the patient metabolic system and, as a result, appears better suited for mitigation of time delays due to subcutaneous glucose sensing and insulin infusion. In addition, MPC is a better platform for incorporation of predictions of the effects of meals and for introduction of constraints on insulin delivery rate and glucose values that safeguard against insulin overdose or extreme blood glucose fluctuations. In some sense, an MPC algorithm works as a chess strategy (Fig. 4). On the basis of past game (glucose) history, a several-moves-ahead strategy (insulin infusion rate) is planned, but only the first move (e.g., the next 15-min insulin infusion) is implemented; after the response of the opponent, the strategy is reassessed, but only the second move (the 30-min insulin infusion rate) is implemented, and so on. In reality glucose prediction may be different from the actual glucose measurement or an unexpected event may happen; with this strategy these events are taken into account in the next plan.
FIG. 4.
A: The concept of MPC. At each step, future glucose levels are predicted and insulin delivery strategy is mapped several steps ahead. Then, the first insulin delivery step is implemented, and the situation is reassessed with new glucose data. The process is very similar to a chess game in which several moves are planned ahead, and after the implementation of the first move the position is reassessed given the response of the opponent. B: The critical stage of the famous chess game between Leonid Stein (white) and Lajos Portisch (black), Stockholm, 1962 (courtesy of Leon Fahri, University of Virginia).
Several successful clinical trials using MPC were recently published. Kovatchev et al. (31) reported a study in which the aggressiveness of the controller was individualized using patient parameters such as body weight, carbohydrate ratio, and insulin basal rate. Hovorka et al. (28) used a multimodel MPC approach, deciding in real time which patient model is best fitting the data in hand, while dual-hormone strategies adding glucagon administration to insulin delivery to avoid hypoglycemia were used by El-Khatib et al. (30) and Castle et al. (105).
Additional difficulties that the control algorithm must face arise from coping with inter- and intrapatient variability. Fortunately, MPC allows for relatively straightforward individualization using patient-specific model parameters (106). Given the difficulty of identifying accurate individual models, a customizable controller has been proposed, individually tuned through a “control aggressiveness” parameter calculated from a few routine biometric and clinical data of each individual (107). In addition, MPC can have “learning” capabilities; it has been shown that a class of algorithms (known as run-to-run control) can “learn” specifics of patients’ daily routine (e.g., timing of meals) and then optimize the response to a subsequent meal using this information (108,109), or account for circadian fluctuation in insulin resistance, such as the dawn phenomenon observed in some people (110).
Finally, an MPC system can also have certain feed-forward capabilities, i.e., the ability to use a combination of feed-forward (e.g., patient-initiated) and feedback (controller-initiated) insulin delivery that can partially solve the dilemma posed by the need for trade-off between slow-pace regulation in quasi-steady state and prompt correction of meals. Associated with such a feed-forward action is a nominal glucose profile, which represents the expected consequence of the conventional patient-initiated therapy. The algorithm bases its actions on the difference between the sensor signal and this nominal profile. If the difference is zero, no closed-loop correction is applied and the patient is subject to the conventional therapy alone. In practice the difference will always be nonzero, thus a feed-forward action would also prompt small-size feedback corrections adapting to unpredicted events, disturbances and changes in patient’s dynamics. Clinical results obtained by this type of control strategy are reported by Kovatchev et al. (31).
A step forward: in silico experiments replacing animal trials
The future development of AP will be greatly accelerated by using mathematical modeling and computer simulation. A number of simulation models have been proposed in the last 4 decades and used to assess the performance of control algorithms and insulin infusion routes (111–117). However, all these models are “average,” meaning that they are only able to simulate average population dynamics but not the interindividual variability. The average-model approach is not sufficient for realistic in silico experimentation with control scenarios. For this purpose, it is necessary to have a simulator equipped with a cohort of in silico subjects that spans sufficiently well the observed interperson variability of key metabolic parameters in the type 1 diabetic population. The knowledge on intersubject variability is indeed crucial to the design of robust controllers, providing valuable information about their safety and limitations.
Building on the large scale meal model developed in the healthy state (116,117), we have developed a type 1 diabetes simulator that, thanks to its ability to realistically describe intersubject variability, has been accepted by the Food and Drug Administration as a substitute of preclinical animal trials for certain insulin treatments (32). In this simulator, a virtual human is described as a combination of several glucose and insulin subsystems. To permit in silico experiments using CGM, the model includes subcutaneous glucose transport and sensor errors. In summary, the model consists of 13 differential equations and 35 parameters for each subject (116,117). The simulator is equipped with 100 virtual adults, 100 adolescents, and 100 children, spanning the variability of type 1 diabetic population observed in vivo. Key “biometric” characteristics of these virtual subjects are presented by Kovatchev et al. (32). Figure 5 illustrates the overall design of the simulation model.
FIG. 5.
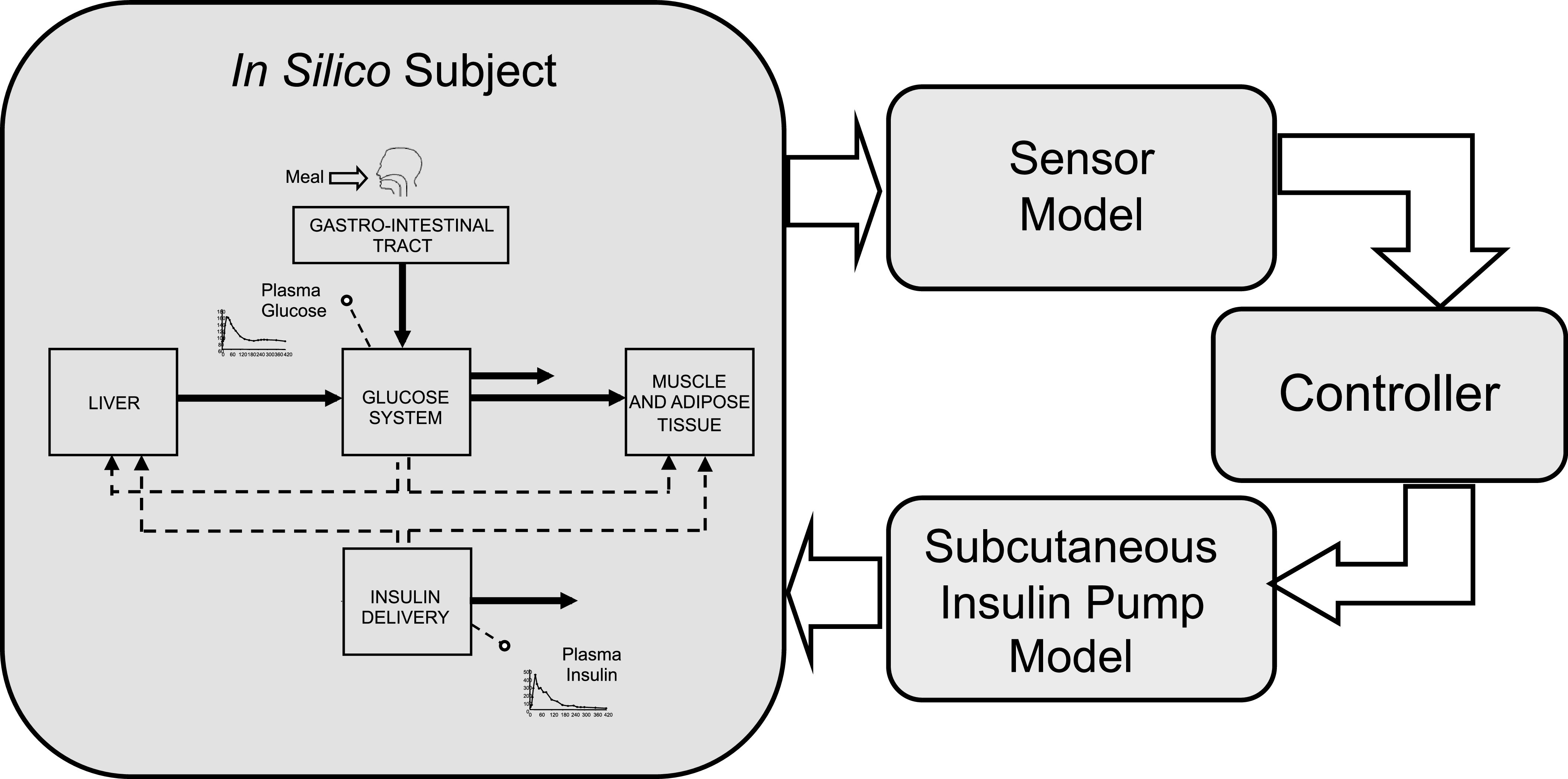
Principal component of the type 1 diabetes simulator: a model of the glucose-insulin system, a model of the sensor, a model of the insulin pump and subcutaneous insulin kinetics, and the controller to be tested.
With this technology, any meal and insulin delivery scenario can be pilot-tested very efficiently in silico, prior to its clinical application. Because in silico experiments produce results at a fraction of time and cost of animal trials, this simulator in now adopted by the JDRF Artificial Pancreas Consortium and by others as a primary test bed for new closed-loop control algorithms. The capabilities of the simulator are now being expanded by incorporating intraday variability of key fluxes (e.g., glucose production) and signals (e.g., insulin sensitivity [118]), and by including hypoglycemia counterregulation (119).
Modular Architecture for Sequential AP Development
Today’s technological advancements open the possibility for ambulatory AP. To account for the multitude of available possibilities, academic, and industrial developments, we have introduced the concept of modular approach to AP design, which allows technologies developed by different entities to be seamlessly integrated in a functional hierarchical system that can be sequentially deployed in clinical and ambulatory studies. Figure 6 presents an outline of this modular-architecture concept.
FIG. 6.
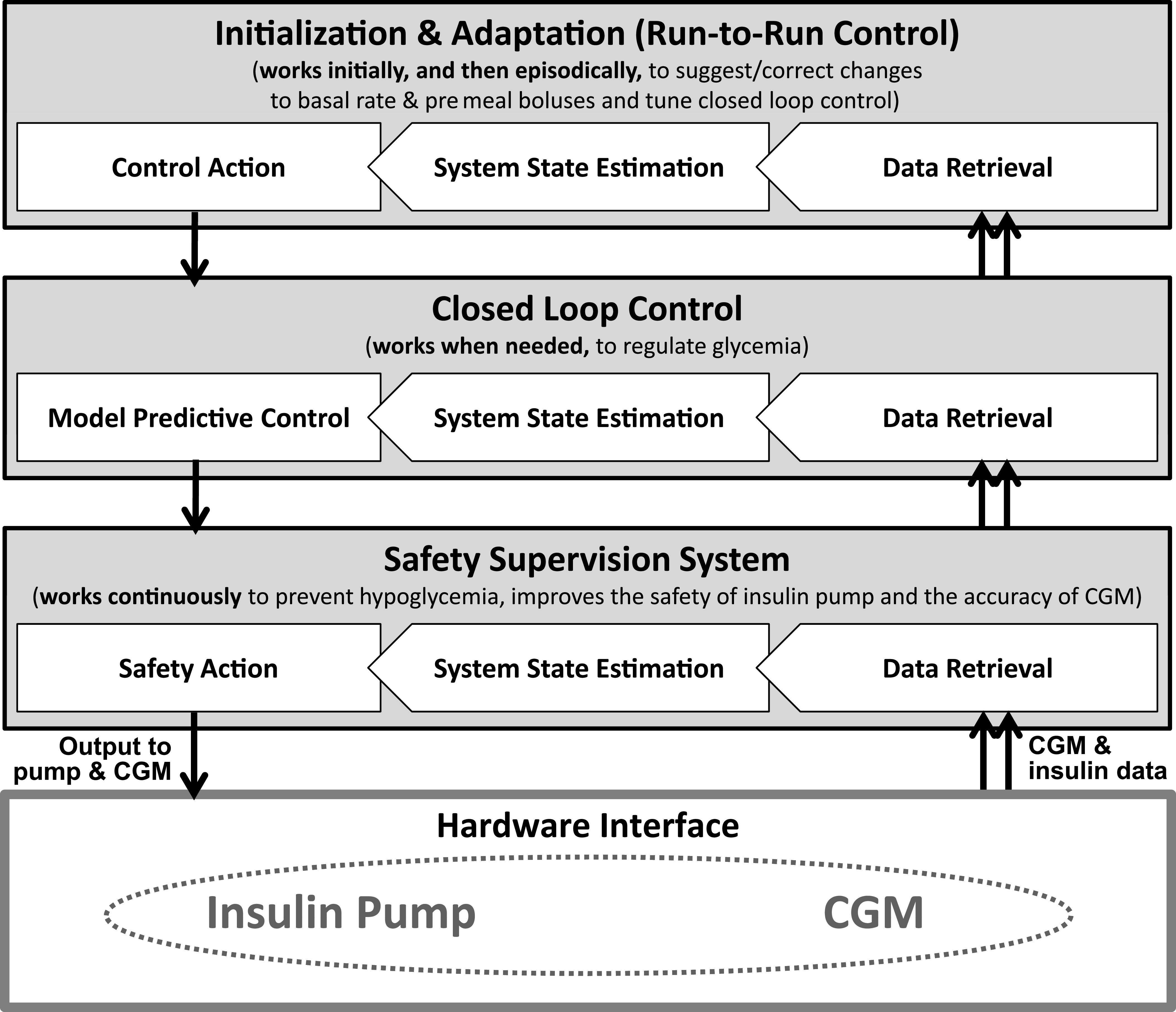
Modular architecture for sequential AP development.
The key advantage of modular AP architecture is the possibility for sequential development, clinical testing, and ambulatory acceptance of elements (modules) of the closed-loop system. In engineering terms, we suggest that the AP should have separate interacting components responsible for prevention of hypoglycemia, postprandial insulin correction boluses, basal rate control, and administration of premeal boluses (120). In this scheme, control modules receive information from system state estimation modules that are responsible for tracking glucose fluctuations and the amount of active insulin at any point in time. This structure is dictated by the natural separation of the computational elements of a closed-loop control system into algorithms estimating the state of the person and algorithms actuating control. The control layers work on different time scales. At the bottom, the fastest layer is in charge of safety requirements. Possible algorithms include pump shutoff (76), insulin on board, and smooth attenuation of the insulin pump (121). Immediately above, there is the real-time control layer deciding insulin delivery based on latest CGM data, previous insulin delivery, and meal information. Typical algorithms are either PID, MPC, or the recently introduced Zone MPC controller (122). The top layer (offline control tuning) is in charge of tuning the real-time control layer using clinical parameters and historical data. Each layer processes available information (CGM and patient inputs) in order to take decisions that are passed to a lower layer. If necessary, commands from an upper layer can be overridden; a typical example is the safety layer canceling insulin delivery suggested by the real-time control module.
With modular architecture in place, various increasingly complex configurations of an AP system become possible. For example, a relatively simple control system responsible only for nighttime basal rate regulation has been successfully tested as a first step to AP (31), followed by control of risk for hypoglycemia associated with exercise (123). More recently, a new modular control-to-range algorithm has been introduced as an adjunct to, not a replacement of, standard basal-bolus pump therapy, intervening only if corrections of hypo- or hyperglycemia are needed (120). This control strategy resulted in reduced average glucose without increasing patients’ risk for hypoglycemia (124).
Further, the progression of AP would entail moving the system to outpatient setting. This critical step would require specific elements, such as server and communication tools for remote monitoring but also for remote intervention. Remote monitoring would be particularly important for the first ambulatory clinical trials that would require continuous “intelligent” observation of AP first deployed outside of the hospital. From there, step-by-step move to home use would follow module-by-module approach under remote monitoring. Finally, fully automated closed-loop is expected to deliver safe and efficacious glucose control at home for a prolonged period of time. To cope with the changing environmental conditions and with the physiological/behavioral changes of the patient, the ambulatory AP will have to adapt to the changes in an individual’s biobehavioral parameters over time. Possible methods to cope with changing reality include individual controller calibration strategies and run-to-run control algorithms (107–110), as well as behavioral analysis and profiling of patient lifestyle (125). Many of these advanced methods are now on the drawing board. Table 1 summarizes the principal components of a closed-loop system, including the CGM, the insulin infusion device, the control algorithm and the associated human factors, and lists the areas that need further development before the ambulatory AP becomes a reality.
TABLE 1.
Components of the AP system and the improvements needed before the ambulatory AP enters mainstream use
| Components | Desirable improvements |
|---|---|
| Glucose sensing | Reliability (minimize missing data) |
| Error (reduce noise and drift, improve calibration) | |
| Durability and wearability | |
| Long-term implantable and noninvasive technologies | |
| Insulin delivery | Insulin pharmacokinetics and pharmacodynamics |
| Reliability of infusion (infusion sets) | |
| Durability and wearability | |
| Alternative routes (intraperitoneal, intradermal, inhaled) | |
| Control algorithm | Model prediction (improve horizon and accuracy) |
| Individualization (prescription of a control algorithm) | |
| Automated meal and exercise recognition and control | |
| Real-time adaptation to patient physiology and behavior | |
| Platform | Communication between devices (first step to integration) |
| Remote monitoring, alerts, and telecommunication | |
| Integration of pump, sensor, and control devices | |
| Integration of sensing and insulin delivery sites | |
| Human factors | Device user interface (typically graphical user interface) |
| Hazard identification and task prioritization | |
| Hazard mitigation and unexpected event control | |
| Human factors validation testing |
ACKNOWLEDGMENTS
This project is supported by the JDRF Artificial Pancreas Project Consortium, the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases Grant RO1 085623, the Italian Ministero dell’Università e della Ricerca PRIN project “Artificial pancreas: physiological models, control algorithms and clinical test” and the European project “Artificial Pancreas at Home (AP@Home).”
No potential conflicts of interest relevant to this article were reported.
C.C., E.R., and B.K. equally contributed to the conception and writing of the manuscript.
C.C. thanks Robert Rizza, Rita Basu, Andy Basu, and Chiara Dalla Man for their important contribution in developing the oral minimal and maximal glucose models. The authors thank William Clarke for his assistance with the historical perspective of this article. The authors also thank all the colleagues of the international Artificial Pancreas study group (iAP: http://www.iAPstudygroup.org/) for stimulating discussions: Marc Breton, Stephen Patek, Colleen Hughes, Stacey Anderson, Sue Brown, and Susan Demartini (University of Virginia); Eyal Dassau, Francis J Doyle III, Benyamin Grosman, and Howard Zisser (University of California Santa Barbara); Andy Basu and Yogish Kudva (Mayo Clinic); Giuseppe De Nicolao, Lalo Magni, Paola Soru, Chiara Toffanin (University of Pavia); Angelo Avogaro, Daniela Brutttomesso, Alberto Maran, Monica Vedovato, Chiara Dalla Man, Simone Del Favero (University of Padova); and Anne Farret and Jerome Place (University of Montpellier).
REFERENCES
- 1.Kadish AH. Automation control of blood sugar. I. A servomechanism for glucose monitoring and control. Am J Med Electron 1964;3:82–86 [PubMed] [Google Scholar]
- 2.Albisser AM, Leibel BS, Ewart TG, Davidovac Z, Botz CK, Zingg W. An artificial endocrine pancreas. Diabetes 1974;23:389–396 [DOI] [PubMed] [Google Scholar]
- 3.Pfeiffer EF, Thum C, Clemens AH. The artificial beta cell—a continuous control of blood sugar by external regulation of insulin infusion (glucose controlled insulin infusion system). Horm Metab Res 1974;6:339–342 [DOI] [PubMed] [Google Scholar]
- 4.Mirouze J, Selam JL, Pham TC, Cavadore D. Evaluation of exogenous insulin homoeostasis by the artificial pancreas in insulin-dependent diabetes. Diabetologia 1977;13:273–278 [DOI] [PubMed] [Google Scholar]
- 5.Kraegen EW, Campbell LV, Chia YO, Meler H, Lazarus L. Control of blood glucose in diabetics using an artificial pancreas. Aust N Z J Med 1977;7:280–286 [DOI] [PubMed] [Google Scholar]
- 6.Shichiri M, Kawamori R, Yamasaki Y, Inoue M, Shigeta Y, Abe H. Computer algorithm for the artificial pancreatic beta cell. Artif Organs 1978;2(Suppl.):247–250 [Google Scholar]
- 7.Clemens AH, Chang PH, Myers RW. The development of Biostator, a glucose controlled insulin infusion system (GCIIS). Horm Metab Res 1977;(Suppl. 7):23–33 [PubMed] [Google Scholar]
- 8.Yatabe T, Yamazaki R, Kitagawa H, et al. The evaluation of the ability of closed-loop glycemic control device to maintain the blood glucose concentration in intensive care unit patients. Crit Care Med 2011;39:575–578 [DOI] [PubMed] [Google Scholar]
- 9.Pickup JC, Keen H, Parsons JA, Alberti KG. Continuous subcutaneous insulin infusion: an approach to achieving normoglycaemia. BMJ 1978;1:204–207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tamborlane WV, Sherwin RS, Genel M, Felig P. Reduction to normal of plasma glucose in juvenile diabetes by subcutaneous administration of insulin with a portable infusion pump. N Engl J Med 1979;300:573–578 [DOI] [PubMed] [Google Scholar]
- 11.Shichiri M, Kawamori R, Yamasaki Y, Hakui N, Abe H. Wearable artificial endocrine pancreas with needle-type glucose sensor. Lancet 1982;2:1129–1131 [DOI] [PubMed] [Google Scholar]
- 12.Hashiguchi Y, Sakakida M, Nishida K, Uemura T, Kajiwara K, Shichiri M. Development of a miniaturized glucose monitoring system by combining a needle-type glucose sensor with microdialysis sampling method. Long-term subcutaneous tissue glucose monitoring in ambulatory diabetic patients. Diabetes Care 1994;17:387–396 [DOI] [PubMed] [Google Scholar]
- 13.Shichiri M, Sakakida M, Nishida K, Shimoda S. Enhanced, simplified glucose sensors: long-term clinical application of wearable artificial endocrine pancreas. Artif Organs 1998;22:32–42 [DOI] [PubMed] [Google Scholar]
- 14.LeBlanc H, Chauvet D, Lombrail P, Robert JJ. Glycemic control with closed-loop intraperitoneal insulin in type I diabetes. Diabetes Care 1986;9:124–128 [DOI] [PubMed] [Google Scholar]
- 15.Renard E. Implantable closed-loop glucose-sensing and insulin delivery: the future for insulin pump therapy. Curr Opin Pharmacol 2002;2:708–716 [DOI] [PubMed] [Google Scholar]
- 16.Renard E, Place J, Cantwell M, Chevassus H, Palerm CC. Closed-loop insulin delivery using a subcutaneous glucose sensor and intraperitoneal insulin delivery: feasibility study testing a new model for the artificial pancreas. Diabetes Care 2010;33:121–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bergman RN, Ider YZ, Bowden CR, Cobelli C. Quantitative estimation of insulin sensitivity. Am J Physiol 1979;236:E667–E677 [DOI] [PubMed] [Google Scholar]
- 18.Broekhuyse HM, Nelson JD, Zinman B, Albisser AM. Comparison of algorithms for the closed-loop control of blood glucose using the artificial beta cell. IEEE Trans Biomed Eng 1981;28:678–687 [DOI] [PubMed] [Google Scholar]
- 19.Cobelli C, Ruggeri A. Evaluation of portal/peripheral route and of algorithms for insulin delivery in the closed-loop control of glucose in diabetes—a modeling study. IEEE Trans Biomed Eng 1983;30:93–103 [DOI] [PubMed] [Google Scholar]
- 20.Salzsieder E, Albrecht G, Fischer U, Freyse EJ. Kinetic modeling of the glucoregulatory system to improve insulin therapy. IEEE Trans Biomed Eng 1985;32:846–855 [DOI] [PubMed] [Google Scholar]
- 21.Brunetti P, Cobelli C, Cruciani P, et al. A simulation study on a self-tuning portable controller of blood glucose. Int J Artif Organs 1993;16:51–57 [PubMed] [Google Scholar]
- 22.Parker RS, Doyle FJ, 3rd, Peppas NA. A model-based algorithm for blood glucose control in type I diabetic patients. IEEE Trans Biomed Eng 1999;46:148–157 [DOI] [PubMed] [Google Scholar]
- 23.Parker RS, Doyle FJ, 3rd, Peppas NA. The intravenous route to blood glucose control. IEEE Eng Med Biol Mag 2001;20:65–73 [DOI] [PubMed] [Google Scholar]
- 24.Bellazzi R, Nucci G, Cobelli C. The subcutaneous route to insulin-dependent diabetes therapy: closed-loop and partially closed-loop control strategies for insulin delivery and measuring glucose concentration. IEEE Eng Med Biol Mag 2001;20:54–64 [DOI] [PubMed] [Google Scholar]
- 25.Steil GM, Rebrin K, Darwin C, Hariri F, Saad MF. Feasibility of automating insulin delivery for the treatment of type 1 diabetes. Diabetes 2006;55:3344–3350 [DOI] [PubMed] [Google Scholar]
- 26.Hovorka R, Canonico V, Chassin LJ, et al. Nonlinear model predictive control of glucose concentration in subjects with type 1 diabetes. Physiol Meas 2004;25:905–920 [DOI] [PubMed] [Google Scholar]
- 27.Weinzimer SA, Steil GM, Swan KL, Dziura J, Kurtz N, Tamborlane WV. Fully automated closed-loop insulin delivery versus semiautomated hybrid control in pediatric patients with type 1 diabetes using an artificial pancreas. Diabetes Care 2008;31:934–939 [DOI] [PubMed] [Google Scholar]
- 28.Hovorka R, Allen JM, Elleri D, et al. Manual closed-loop insulin delivery in children and adolescents with type 1 diabetes: a phase 2 randomised crossover trial. Lancet 2010;375:743–751 [DOI] [PubMed] [Google Scholar]
- 29.Hovorka R, Kumareswaran K, Harris J, Allen JM, Elleri D, Xing D, et al. Overnight closed loop insulin delivery (artificial pancreas) in adults with type 1 diabetes: crossover randomised controlled studies. BMJ 2011;342:d1855 [DOI] [PMC free article] [PubMed]
- 30.El-Khatib FH, Russell SJ, Nathan DM, Sutherlin RG, Damiano ER. A bihormonal closed-loop artificial pancreas for type 1 diabetes. Sci Transl Med 2010;2:27ra27 [DOI] [PMC free article] [PubMed]
- 31.Kovatchev BP, Cobelli C, Renard E, et al. Multinational study of subcutaneous model-predictive closed-loop control in type 1 diabetes mellitus: summary of the results. J Diabetes Sci Technol 2010;4:1374–1381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kovatchev BP, Breton MD, Man CD, Cobelli C. In silico preclinical trials: a proof of concept in closed-loop control of type 1 diabetes. J Diabetes Sci Tech 2009;3:44–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dassau E, Zisser H, Palerm CC, Buckingham BA, Jovanovič L, Doye III FJ. Modular artificial β-cell system: a prototype for clinical research. J Diabetes Sci Technol 2008;2:863-872 [DOI] [PMC free article] [PubMed]
- 34.Mastrototaro JJ. The MiniMed continuous glucose monitoring system. Diabetes Technol Ther 2000;2(Suppl. 1):S13–S18 [DOI] [PubMed] [Google Scholar]
- 35.Bode BW. Clinical utility of the continuous glucose monitoring system. Diabetes Technol Ther 2000;2(Suppl. 1):S35–S41 [DOI] [PubMed] [Google Scholar]
- 36.Diabetes Research in Children Network (DIRECNET) Study Group. The accuracy of the CGMS in children with type 1 diabetes: results of the diabetes research in children network (DirecNet) accuracy study. Diabetes Technol Ther 2003;5:781–789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feldman B, Brazg R, Schwartz S, Weinstein R. A continuous glucose sensor based on wired enzyme technology — results from a 3-day trial in patients with type 1 diabetes. Diabetes Technol Ther 2003;5:769–779 [DOI] [PubMed] [Google Scholar]
- 38.Garg S, Zisser H, Schwartz S, et al. Improvement in glycemic excursions with a transcutaneous, real-time continuous glucose sensor: a randomized controlled trial. Diabetes Care 2006;29:44–50 [DOI] [PubMed] [Google Scholar]
- 39.Kovatchev BP, Anderson SM, Heinemann L, Clarke WL. Comparison of the numerical and clinical accuracy of four continuous glucose monitors. Diabetes Care 2008;31:1160–1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Deiss D, Bolinder J, Riveline JP, et al. Improved glycemic control in poorly controlled patients with type 1 diabetes using real-time continuous glucose monitoring. Diabetes Care 2006;29:2730–2732 [DOI] [PubMed] [Google Scholar]
- 41.Kovatchev BP, Clarke WL. Continuous glucose monitoring reduces risks for hypo- and hyperglycemia and glucose variability in diabetes. Diabetes 2007;56(Suppl. 1):A23
- 42.Tamborlane WV, Beck RW, Bode BW, et al. ; Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 2008;359:1464–1476 [DOI] [PubMed] [Google Scholar]
- 43.Klonoff DC. Continuous glucose monitoring: roadmap for 21st century diabetes therapy. Diabetes Care 2005;28:1231–1239 [DOI] [PubMed] [Google Scholar]
- 44.Hirsch IB, Armstrong D, Bergenstal RM, et al. Clinical application of emerging sensor technologies in diabetes management: consensus guidelines for continuous glucose monitoring (CGM). Diabetes Technol Ther 2008;10:232–244; quiz 245–246 [DOI] [PubMed] [Google Scholar]
- 45.Hovorka R. Continuous glucose monitoring and closed-loop systems. Diabet Med 2006;23:1–12 [DOI] [PubMed] [Google Scholar]
- 46.Klonoff DC. The artificial pancreas: how sweet engineering will solve bitter problems. J Diabetes Sci Tech 2007;1:72–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rebrin K, Steil GM, van Antwerp WP, Mastrototaro JJ. Subcutaneous glucose predicts plasma glucose independent of insulin: implications for continuous monitoring. Am J Physiol 1999;277:E561–E571 [DOI] [PubMed] [Google Scholar]
- 48.Rebrin K, Steil GM. Can interstitial glucose assessment replace blood glucose measurements? Diabetes Technol Ther 2000;2:461–472 [DOI] [PubMed] [Google Scholar]
- 49.Steil GM, Rebrin K, Hariri F, et al. Interstitial fluid glucose dynamics during insulin-induced hypoglycaemia. Diabetologia 2005;48:1833–1840 [DOI] [PubMed] [Google Scholar]
- 50.Knobbe EJ, Buckingham B. The extended Kalman filter for continuous glucose monitoring. Diabetes Technol Ther 2005;7:15–27 [DOI] [PubMed] [Google Scholar]
- 51.King C, Anderson SM, Breton M, Clarke WL, Kovatchev BP. Modeling of calibration effectiveness and blood-to-interstitial glucose dynamics as potential confounders of the accuracy of continuous glucose sensors during hyperinsulinemic clamp. J Diabetes Sci Tech 2007;1:317–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Buckingham BA, Kollman C, Beck R, et al. ; Diabetes Research In Children Network (Direcnet) Study Group. Evaluation of factors affecting CGMS calibration. Diabetes Technol Ther 2006;8:318–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuure-Kinsey M, Palerm CC, Bequette BW. A dual-rate Kalman filter for continuous glucose monitoring. In Proceedings of the IEEE Engineering in Medicine and Biology Society, IEEE Engineering in Medicine and Biology Society, New York, 2006; p. 63-66 [DOI] [PubMed] [Google Scholar]
- 54.Facchinetti A, Sparacino G, Cobelli C. Enhanced accuracy of continuous glucose monitoring by online extended kalman filtering. Diabetes Technol Ther 2010;12:353–363 [DOI] [PubMed] [Google Scholar]
- 55.Aussedat B, Dupire-Angel M, Gifford R, Klein JC, Wilson GS, Reach G. Interstitial glucose concentration and glycemia: implications for continuous subcutaneous glucose monitoring. Am J Physiol Endocrinol Metab 2000;278:E716–E728 [DOI] [PubMed] [Google Scholar]
- 56.Kovatchev BP, Clarke WL. Peculiarities of the continuous glucose monitoring data stream and their impact on developing closed-loop control technology. J Diabetes Sci Tech 2008;2:158–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Boyne MS, Silver DM, Kaplan J, Saudek CD. Timing of changes in interstitial and venous blood glucose measured with a continuous subcutaneous glucose sensor. Diabetes 2003;52:2790–2794 [DOI] [PubMed] [Google Scholar]
- 58.Kulcu E, Tamada JA, Reach G, Potts RO, Lesho MJ. Physiological differences between interstitial glucose and blood glucose measured in human subjects. Diabetes Care 2003;26:2405–2409 [DOI] [PubMed] [Google Scholar]
- 59.Stout PJ, Racchini JR, Hilgers ME. A novel approach to mitigating the physiological lag between blood and interstitial fluid glucose measurements. Diabetes Technol Ther 2004;6:635–644 [DOI] [PubMed] [Google Scholar]
- 60.Wentholt IME, Hart AAM, Hoekstra JBL, Devries JH. Relationship between interstitial and blood glucose in type 1 diabetes patients: delay and the push-pull phenomenon revisited. Diabetes Technol Ther 2007;9:169–175 [DOI] [PubMed] [Google Scholar]
- 61.Facchinetti A, Sparacino G, Cobelli C. Modeling the error of continuous glucose monitoring sensor data: critical aspects discussed through simulation studies. J Diabetes Sci Tech 2010;4:4–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Clarke WL, Kovatchev BP. Continuous glucose sensors: continuing questions about clinical accuracy. J Diabetes Sci Technol 2007;1:164–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Diabetes Research in Children Network (DirecNet) Study Group. The accuracy of the Guardian RT continuous glucose monitor in children with type 1 diabetes. Diabetes Technol Ther 2008;10:266–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Garg SK, Smith J, Beatson C, Lopez-Baca B, Voelmle M, Gottlieb PA. Comparison of accuracy and safety of the SEVEN and the Navigator continuous glucose monitoring systems. Diabetes Technol Ther 2009;11:65–72 [DOI] [PubMed] [Google Scholar]
- 65.Poscia A, Mascini M, Moscone D, et al. A microdialysis technique for continuous subcutaneous glucose monitoring in diabetic patients (part 1). Biosens Bioelectron 2003;18:891–898 [DOI] [PubMed] [Google Scholar]
- 66.Feldman BJ, McGarraugh GV. Method of calibrating an analyte measurement device, and associated methods, devices and systems. U.S. Patent 7,299,082. 20 November 2007
- 67.Simpson P, Brister M, Wightlin M, Pryor J. Dual electrode system for a continuous analyte sensor. World Intellectual Property Organization. Publication number WO/2008/042918. 10 April 2008
- 68.Chase JG, Hann CE, Jackson M, et al. Integral-based filtering of continuous glucose sensor measurements for glycaemic control in critical care. Comput Methods Programs Biomed 2006;82:238–247 [DOI] [PubMed] [Google Scholar]
- 69.Palerm CC, Willis JP, Desemone J, Bequette BW. Hypoglycemia prediction and detection using optimal estimation. Diabetes Technol Ther 2005;7:3–14 [DOI] [PubMed] [Google Scholar]
- 70.Facchinetti A, Sparacino G, Cobelli C. An online self-tunable method to denoise CGM sensor data. IEEE Trans Biomed Eng 2010;57:634–641 [DOI] [PubMed] [Google Scholar]
- 71.Heise T, Koschinsky T, Heinemann L, Lodwig V; Glucose Monitoring Study Group. Hypoglycemia warning signal and glucose sensors: requirements and concepts. Diabetes Technol Ther 2003;5:563–571 [DOI] [PubMed] [Google Scholar]
- 72.Bode B, Gross K, Rikalo N, et al. Alarms based on real-time sensor glucose values alert patients to hypo- and hyperglycemia: the guardian continuous monitoring system. Diabetes Technol Ther 2004;6:105–113 [DOI] [PubMed] [Google Scholar]
- 73.McGarraugh G, Bergenstal R. Detection of hypoglycemia with continuous interstitial and traditional blood glucose monitoring using the FreeStyle Navigator Continuous Glucose Monitoring System. Diabetes Technol Ther 2009;11:145–150 [DOI] [PubMed] [Google Scholar]
- 74.Noujaim SE, Horwitz D, Sharma M, Marhoul J. Accuracy requirements for a hypoglycemia detector: an analytical model to evaluate the effects of bias, precision, and rate of glucose change. J Diabetes Sci Technol 2007;1:653–668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ward WK. The role of new technology in the early detection of hypoglycemia. Diabetes Technol Ther 2004;6:115–117 [DOI] [PubMed] [Google Scholar]
- 76.Buckingham B, Cobry E, Clinton P, et al. Preventing hypoglycemia using predictive alarm algorithms and insulin pump suspension. Diabetes Technol Ther 2009;11:93–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Selam JL, Charles MA. Devices for insulin administration. Diabetes Care 1990;13:955–979 [DOI] [PubMed] [Google Scholar]
- 78.Blackshear PJ, Shulman GI, Roussell AM, et al. Metabolic response to three years of continuous, basal rate intravenous insulin infusion in type II diabetic patients. J Clin Endocrinol Metab 1985;61:753–760 [DOI] [PubMed] [Google Scholar]
- 79.Selam JL, Micossi P, Dunn FL, Nathan DM. Clinical trial of programmable implantable insulin pump for type I diabetes. Diabetes Care 1992;15:877–885 [DOI] [PubMed] [Google Scholar]
- 80.Nelson JA, Stephen R, Landau ST, Wilson DE, Tyler FH. Intraperitoneal insulin administration produces a positive portal-systemic blood insulin gradient in unanesthetized, unrestrained swine. Metabolism 1982;31:969–972 [DOI] [PubMed] [Google Scholar]
- 81.Botz CK, Leibel BS, Zingg W, Gander RE, Albisser AM. Comparison of peripheral and portal routes of insulin infusion by a computer-controlled insulin infusion system (artificial endocrine pancreas). Diabetes 1976;25:691–700 [DOI] [PubMed] [Google Scholar]
- 82.Giacca A, Caumo A, Galimberti G, et al. Peritoneal and subcutaneous absorption of insulin in type I diabetic subjects. J Clin Endocrinol Metab 1993;77:738–742 [DOI] [PubMed] [Google Scholar]
- 83.Nathan DM, Dunn FL, Bruch J, et al. Postprandial insulin profiles with implantable pump therapy may explain decreased frequency of severe hypoglycemia, compared with intensive subcutaneous regimens, in insulin-dependent diabetes mellitus patients. Am J Med 1996;100:412–417 [DOI] [PubMed] [Google Scholar]
- 84.Selam JL, Raymond M, Jacquemin JL, Orsetti A, Richard JL, Mirouze J. Pharmacokinetics of insulin infused intra-peritoneally via portable pumps. Diabete Metab 1985;11:170–173 [PubMed] [Google Scholar]
- 85.Oskarsson PR, Lins PE, Backman L, Adamson UC. Continuous intraperitoneal insulin infusion partly restores the glucagon response to hypoglycaemia in type 1 diabetic patients. Diabetes Metab 2000;26:118–124 [PubMed] [Google Scholar]
- 86.Oskarsson PR, Lins PE, Wallberg Henriksson H, Adamson UC. Metabolic and hormonal responses to exercise in type 1 diabetic patients during continuous subcutaneous, as compared to continuous intraperitoneal, insulin infusion. Diabetes Metab 1999;25:491–497 [PubMed] [Google Scholar]
- 87.Saudek CD, Selam JL, Pitt HA, et al. A preliminary trial of the programmable implantable medication system for insulin delivery. N Engl J Med 1989;321:574–579 [DOI] [PubMed] [Google Scholar]
- 88.Hanaire-Broutin H, Broussolle C, Jeandidier N, et al. ; The EVADIAC Study Group. Feasibility of intraperitoneal insulin therapy with programmable implantable pumps in IDDM. A multicenter study. The EVADIAC Study Group. Evaluation dans le Diabète du Traitement par Implants Actifs. Diabetes Care 1995;18:388–392 [DOI] [PubMed] [Google Scholar]
- 89.Catargi B, Meyer L, Melki V, Renard E, Jeandidier N; for the EVADIAC Study Group. Comparison of blood glucose stability and HbA1C between implantable insulin pumps using U400 HOE 21PH insulin and external pumps using lispro in type 1 diabetic patients: a pilot study. Diabetes Metab 2002;28:133–137 [PubMed] [Google Scholar]
- 90.Broussolle C, Jeandidier N, Hanaire-Broutin H; The EVADIAC Study Group. Evaluation of Active Implants in Diabetes Society. French multicentre experience of implantable insulin pumps. Lancet 1994;343:514–515 [DOI] [PubMed] [Google Scholar]
- 91.Renard E, Bouteleau S, Jacques-Apostol D, et al. Insulin underdelivery from implanted pumps using peritoneal route. Determinant role of insulin pump compatibility. Diabetes Care 1996;19:812–817 [DOI] [PubMed] [Google Scholar]
- 92.Olsen CL, Chan E, Turner DS, et al. Insulin antibody responses after long-term intraperitoneal insulin administration via implantable programmable insulin delivery systems. Diabetes Care 1994;17:169–176 [DOI] [PubMed] [Google Scholar]
- 93.Renard E, Costalat G, Chevassus H, Bringer J. Artificial beta-cell: clinical experience toward an implantable closed-loop insulin delivery system. Diabetes Metab 2006;32:497–502 [DOI] [PubMed] [Google Scholar]
- 94.Shishko PI, Kovalev PA, Goncharov VG, Zajarny IU. Comparison of peripheral and portal (via the umbilical vein) routes of insulin infusion in IDDM patients. Diabetes 1992;41:1042–1049 [DOI] [PubMed] [Google Scholar]
- 95.Pickup J, Keen H. Continuous subcutaneous insulin infusion at 25 years: evidence base for the expanding use of insulin pump therapy in type 1 diabetes. Diabetes Care 2002;25:593–598 [DOI] [PubMed] [Google Scholar]
- 96.Zisser H, Jovanovic L. OmniPod Insulin Management System: patient perceptions, preference, and glycemic control. Diabetes Care 2006;29:2175. [DOI] [PubMed] [Google Scholar]
- 97.Howey DC, Bowsher RR, Brunelle RL, Woodworth JR. [Lys(B28), Pro(B29)]-human insulin. A rapidly absorbed analogue of human insulin. Diabetes 1994;43:396–402 [DOI] [PubMed] [Google Scholar]
- 98.Melki V, Renard E, Lassmann-Vague V, et al. Improvement of HbA1c and blood glucose stability in IDDM patients treated with lispro insulin analog in external pumps. Diabetes Care 1998;21:977–982 [DOI] [PubMed] [Google Scholar]
- 99.Renard E, Guerci B, Leguerrier AM, Boizel R; Accu-Chek FlexLink Study Group. Lower rate of initial failures and reduced occurrence of adverse events with a new catheter model for continuous subcutaneous insulin infusion: prospective, two-period, observational, multicenter study. Diabetes Technol Ther 2010;12:769–773 [DOI] [PubMed] [Google Scholar]
- 100.Guerci B, Meyer L, Sallé A, et al. Comparison of metabolic deterioration between insulin analog and regular insulin after a 5-hour interruption of a continuous subcutaneous insulin infusion in type 1 diabetic patients. J Clin Endocrinol Metab 1999;84:2673–2678 [DOI] [PubMed] [Google Scholar]
- 101.Steil GM, Panteleon AE, Rebrin K. Closed-loop insulin delivery-the path to physiological glucose control. Adv Drug Deliv Rev 2004;56:125–144 [DOI] [PubMed] [Google Scholar]
- 102.Bequette BW. A critical assessment of algorithms and challenges in the development of a closed-loop artificial pancreas. Diabetes Technol Ther 2005;7:28–47 [DOI] [PubMed] [Google Scholar]
- 103.Cobelli C, Man CD, Sparacino G, Magni L, De Nicolao G, Kovatchev BP. Diabetes: models, signals, and control. IEEE Rev Biomed Eng 2009;2:54–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Palerm CC. Physiologic insulin delivery with insulin feedback: a control systems perspective. Comput Methods Programs Biomed 2011;102:130–137 [DOI] [PubMed] [Google Scholar]
- 105.Castle JR, Engle JM, El Youssef J, et al. Novel use of glucagon in a closed-loop system for prevention of hypoglycemia in type 1 diabetes. Diabetes Care 2010;33:1282–1287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Magni L, Raimondo DM, Bossi L, et al. Model predictive control of type 1 diabetes: an in silico trial. J Diabetes Sci Tech 2007;1:804–812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Magni L, Forgione M, Toffanin C, et al. Run-to-run tuning of model predictive control for type 1 diabetes subjects: in silico trial. J Diabetes Sci Tech 2009;3:1091–1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zisser H, Jovanovic L, Doyle FJ, 3rd, Ospina P, Owens C. Run-to-run control of meal-related insulin dosing. Diabetes Technol Ther 2005;7:48–57 [DOI] [PubMed] [Google Scholar]
- 109.Owens C, Zisser H, Jovanovic L, Srinivasan B, Bonvin D, Doyle FJ, 3rd. Run-to-run control of blood glucose concentrations for people with Type 1 diabetes mellitus. IEEE Trans Biomed Eng 2006;53:996–1005 [DOI] [PubMed] [Google Scholar]
- 110.Palerm CC, Zisser H, Jovanovič L, Doyle FJ, 3rd. A Run-to-Run Control Strategy to Adjust Basal Insulin Infusion Rates in Type 1 Diabetes. J Process Contr 2008;18:258–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Srinivasan R, Kadish AH, Sridhar R. A mathematical model for the control mechanism of free fatty acid-glucose metabolism in normal humans. Comput Biomed Res 1970;3:146–165 [DOI] [PubMed] [Google Scholar]
- 112.Cobelli C, Ruggeri A. Evaluation of alternative model structures of metabolic systems: two case studies on model identification and validation. Med Biol Eng Comput 1982;20:444–450 [DOI] [PubMed] [Google Scholar]
- 113.Cobelli C, Mari A. Validation of mathematical models of complex endocrine-metabolic systems. A case study on a model of glucose regulation. Med Biol Eng Comput 1983;21:390–399 [DOI] [PubMed] [Google Scholar]
- 114.Lehmann ED, Deutsch T. A physiological model of glucose-insulin interaction in type 1 diabetes mellitus. J Biomed Eng 1992;14:235–242 [DOI] [PubMed] [Google Scholar]
- 115.Andreassen S, Benn JJ, Hovorka R, Olesen KG, Carson ER. A probabilistic approach to glucose prediction and insulin dose adjustment: description of metabolic model and pilot evaluation study. Comput Methods Programs Biomed 1994;41:153–165 [DOI] [PubMed] [Google Scholar]
- 116.Dalla Man C, Rizza RA, Cobelli C. Meal simulation model of the glucose-insulin system. IEEE Trans Biomed Eng 2007;54:1740–1749 [DOI] [PubMed] [Google Scholar]
- 117.Dalla Man Raimondo DM, Rizza RA, Cobelli C. GIM, simulation software of meal glucose-insulin model. J Diabetes Sci Technol 2007;1:323–330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Saad A, Dalla Man C, Debashis N, et al. Diurnal pattern in insulin action, secretion and hepatic extraction in halthy humans: implications for artificial pancreas software. Diabetes 2011;60(Suppl. 1):A94 [Google Scholar]
- 119.Micheletto F, Dalla Man C, Vella A, Cobelli C. A model of glucagon secretion and action in healthy subjects. Proceedings of the 10th Diabetes Technology Meeting, Bethesda, MD, 2010, A105 [Google Scholar]
- 120.Kovatchev BP, Patek SD, Dassau E, et al. ; Juvenile Diabetes Research Foundation Artificial Pancreas Consortium. Control to range for diabetes: functionality and modular architecture. J Diabetes Sci Tech 2009;3:1058–1065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hughes CS, Patek SD, Breton MD, Kovatchev BP. Hypoglycemia prevention via pump attenuation and red-yellow-green “traffic” lights using continuous glucose monitoring and insulin pump data. J Diabetes Sci Technol 2010;4:1146–1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Grosman B, Dassau E, Zisser H, Jovanovič L, Doyle FJ., III Zone model predictive control: a strategy to minimize hyper and hypoglycemic events. J Diabetes Sci Technol 2010;4:961–975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Breton MD, Patek SD, Demartini S, et al. Modular advisory/automated control (AAC) reduces glucose excursions out of a safe range and hypoglycemia in adults & adolescents with Type 1 diabetes. Diabetes 2011;60(Suppl. 1):A41 [Google Scholar]
- 124.Renard E, Bruttomesso D, Magni L, et al. The multi-modular Model Predictive Control-To-Range (MPC2R) allows simultaneous improvement in safety and efficacy of closed-loop insulin delivery in type 1 diabetes (T1D). Diabetes 2011;60(Suppl. 1):A42 [Google Scholar]
- 125.Hughes CS, Patek SD, Breton MD, Kovatchev BP. Anticipating the next meal using meal behavioral profiles: a hybrid model-based stochastic predictive control algorithm for T1DM. Comput Methods Programs Biomed 2011;102:138–148 [DOI] [PMC free article] [PubMed] [Google Scholar]