Key Points
Question
Are levels of preoperative hemoglobin A1c or early postoperative glucose more useful at predicting postoperative complications and readmission following gastrointestinal surgery?
Findings
This retrospective observational cohort study of 23 094 operations at 117 Veterans Affairs medical centers found that peak postoperative glucose levels of less than 250 mg/dL were significantly associated with increased 30-day readmissions. By contrast, preoperative hemoglobin A1c of more than 6.5% was significantly associated with decreased 30-day readmissions.
Meaning
Increased glycemic monitoring and the early treatment of hyperglycemia to maintain peak blood glucose levels of less than 250 mg/dL during the early postoperative period may minimize a patient’s risk of developing complications and being readmitted after undergoing gastrointestinal surgery.
Abstract
Importance
Preoperative hyperglycemia is associated with adverse postoperative outcomes among patients who undergo surgery. Whether preoperative hemoglobin A1c (HbA1c) or postoperative glucose levels are more useful in predicting adverse events following surgery is uncertain in the current literature.
Objective
To examine the use of preoperative HbA1c and early postoperative glucose levels for predicting postoperative complications and readmission.
Design, Setting, and Participants
In this observational cohort study, inpatient gastrointestinal surgical procedures performed at 117 Veterans Affairs hospitals from 2007 to 2014 were identified, and cases of known infection within 3 days before surgery were excluded. Preoperative HbA1c levels were examined as a continuous and categorical variable (<5.7%, 5.7%-6.5%, and >6.5%). A logistic regression modeled postoperative complications and readmissions with the closest preoperative HbA1c within 90 days and the highest postoperative glucose levels within 48 hours of undergoing surgery.
Main Outcomes and Measures
Postoperative complications and 30-day unplanned readmission following discharge.
Results
Of 21 541 participants, 1193 (5.5%) were women, and the mean (SD) age was 63.7 (10.6) years. The cohort included 23 094 operations with measurements of preoperative HbA1c levels and postoperative glucose levels. The complication and 30-day readmission rates were 27.2% and 14.7%, respectively. In logistic regression models adjusting for HbA1c, postoperative glucose levels, postoperative insulin use, diabetes, body mass index (calculated as weight in kilograms divided by height in meters squared), and other patient and procedural factors, peak postoperative glucose levels of more than 250 mg/dL were associated with increased 30-day readmissions (odds ratio, 1.18; 95% CI, 0.99-1.41; P = .07). By contrast, a preoperative HbA1c of more than 6.5% was associated with decreased 30-day readmissions (odds ratio, 0.85; 95% CI, 0.74-0.96; P = .01). As preoperative HbA1c increased, the frequency of 48-hour postoperative glucose checks increased (4.92, 6.89, and 9.71 for an HbA1c <5.7%, 5.7%-6.4%, and >6.5%, respectively; P < .001). Patients with a preoperative HbA1c of more than 6.5% had lower thresholds for postoperative insulin use.
Conclusions and Relevance
Early postoperative hyperglycemia was associated with increased readmission, but elevated preoperative HbA1c was not. A higher preoperative HbA1c was associated with increased postoperative glucose level checks and insulin use, suggesting that heightened postoperative vigilance and a lower threshold to treat hyperglycemia may explain this finding.
This cohort study examines the association between hemoglobin A1c and hospital readmissions among surgical patients with hyperglycemia.
Introduction
Perioperative hyperglycemia is common among surgical patients and has been associated with adverse outcomes.1 Chronic hyperglycemia causes hemoglobin glycation and can be measured by hemoglobin A1c (HbA1c), which reflects the mean glucose level for the previous 120 days.2 The American Diabetic Association uses HbA1c levels of 5.7% to 6.4% and more than 6.5% for diagnosing prediabetes and diabetes, respectively.3 Patients with elevated HbA1c experienced more postoperative infections and longer hospital stays.4,5 Hemoglobin A1c can also be used to identify patients who are at an increased risk for developing acute postoperative hyperglycemia,6 which has also been linked to postoperative complications, including surgical site infections, an increased length of hospital stay, and mortality.7,8,9,10,11,12,13,14
The current literature lacks consensus on whether preoperative HbA1c or postoperative hyperglycemia is more useful for predicting adverse events following surgery.12,15,16,17 In addition, much of the literature pertains to cardiac surgery, which represents a unique patient population that may not be generalizable to patients undergoing gastrointestinal surgery who are at a higher risk for developing postoperative infections. Finally, to our knowledge, while the relationship between perioperative hyperglycemia and postoperative complications has been examined, the effect of this relationship on readmission is largely unknown.
We examined the use of preoperative HbA1c and early postoperative glucose levels for predicting postoperative complications and readmission. We hypothesized that postoperative glucose level measurements in patients with elevated preoperative HbA1c are more vigilantly monitored with a lower threshold of hyperglycemia for insulin treatment. We thereby assessed postoperative glucose level surveillance and insulin treatment among patients with different ranges of preoperative HbA1c. We hypothesized that elevated early postoperative glucose levels would have greater use than preoperative HbA1c for predicting complications and increased readmissions.
Methods
We conducted a secondary analysis of the Veteran Affairs Surgical Quality Improvement Program (VASQIP) database to perform a retrospective observational study of the relationship between preoperative HbA1c, perioperative glucose levels, postoperative complications, and 30-day readmissions. The study protocol was reviewed and approved by the VA Central institutional review board with a waiver of informed consent granted. The Strengthening of Observational Study Designs in Epidemiology checklist was followed.
Study Population
The study population includes a subset of patients who were experiencing inpatient digestive surgeries (principal Current Procedural Terminology codes 40000-49999) at a Veterans Healthcare Administration hospital between October 1, 2007, and September 31, 2014, and who were assessed by VASQIP. Initially, 350 593 unique hospital stays involving a VASQIP-assessed surgery were identified by VASQIP. Eligible surgeries were limited to digestive surgeries only by their principal Current Procedural Terminology code (40000-49999). Patients were excluded from the analysis if they had experienced a documented preoperative infection or infectious complication during the 96 hours immediately following their operation. Patients were also excluded from the analysis if they were missing a postoperative glucose level assessment or preoperative HbA1c assessment. The final analytic sample included 23 094 unique hospital stays involving at least 1 VASQIP-assessed surgical procedure (Figure 1). The unit of analysis for this study was the index surgical procedure. If a patient had undergone more than 1 digestive surgery during a hospitalization, only the procedural characteristics of the first surgery were included in the analysis.
Figure 1. Study Flowchart.
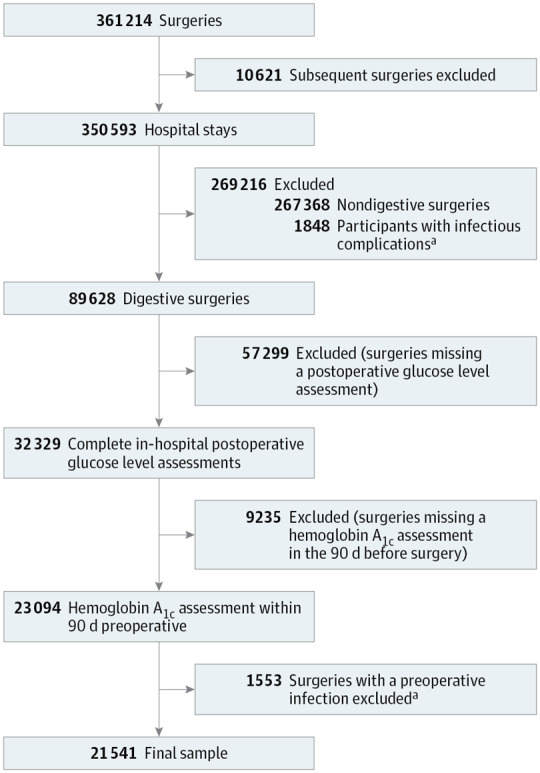
aAll preoperative infectious complications were excluded as well as the infectious complications that occurred in the 96 hours postoperatively.
Data Sources
The covariates of interest included in this analysis were collected from the VASQIP, the VA Decision Support System (DSS), and the VA Corporate Data Warehouse Inpatient data domains. Preoperative, operative, and postoperative characteristics were obtained from VASQIP. The VA Surgical Quality Improvement Program collects these characteristics via a trained nurse abstractor, thus ensuring the reliability of the variables collected.18 Inpatient administrations of insulin in the postoperative period were identified within the DSS pharmacy data. Insulin use in the postoperative period was defined as any administration of insulin during the 48 hours following an operation.
Variables
The main exposure of interest was the closest preoperative HbA1c in the 90 days before a hospital admission as assessed by DSS (DSS laboratory result number, 17) and the highest postoperative glucose level during the 48 hours following an operation (DSS laboratory result number of 10 or 57). Hemoglobin A1c was collected as a continuous variable and categorized as normal (<5.7%), prediabetic (5.7%-6.4%), or diabetic (>6.4%). These categories correspond to a 90-day preoperative mean glucose level of less than 117, 117 to 137, and more than 137 mg/dL, respectively. The peak glucose level was also collected as a continuous variable and examined as a 4-category variable for ease of interpretation (<120, 120-179, 180-250, and >250) after carefully examining trends between glucose as a continuous variable and each of the outcomes examined. In addition to the glucose result, the frequency of glucose level checks was also calculated as the total number of all completed glucose results during the 48 hours following an operation. We limited the postoperative setting to 48 hours to minimize the effect of postoperative events on our outcomes.
The covariates of age, sex, body mass index (BMI) (calculated as weight in kilograms divided by height in meters squared), American Society of Anesthesiologists (ASA) classification, preoperative HbA1c, preoperative glucose level, peak postoperative glucose level, emergency case status, and postoperative length of stay were selected a priori because they are significant predictors for and markers of readmission.19 All variables, with the exception of race/ethnicity and ASA classification, were complete. While ASA classification was only missing for 4 patients (0.02%), race/ethnicity was missing for 3016 patients (14.8%). Race/ethnicity was not a statistically significant predictor of any of the outcomes and thus an unlikely confounder. Notably, when race/ethnicity was tested we found no evidence of collinearity between preoperative diabetes, postoperative blood glucose, and postoperative insulin use. Furthermore, there was no change in the interpretation of results when the variables were removed from the models.
The main outcome of interest was postdischarge readmission or the development of an infection-related postoperative complication as identified by VASQIP. While postoperative infections (a wound infection, pneumonia, urinary tract infecgtion, or sepsis) are not mutually exclusive, they were counted only once in the overall postoperative complications variable. We excluded all patients with a known infection preoperatively and for 96 hours postoperatively to minimize the likelihood that hyperglycemia during the first 48 hours reflected an ongoing infection. Inpatient readmissions in the 30 days following a hospital discharge were identified using the Corporate Data Warehouse Inpatient data domain.
Statistical Analysis
Univariate and bivariate statistics were used to examine the population and compare patients in terms of diabetes status. Univariate and bivariate differences in postoperative outcomes were examined by HbA1c categories, glucose categories, and insulin use. In unadjusted analyses, χ2 tests or Kruskal-Wallis tests were used to test for differences across the groups. Smoothed plots were developed to examine changes in event rates across preoperative HbA1c values. Logistic models adjusting for clinically relevant preoperative and operative characteristics were used to calculate the odds of each outcome across categories of preoperative HbA1c and postoperative glucose. Preoperative HbA1c was added to the adjusted peak 48-hour glucose levels model to understand the contribution of peak 48-hour glucose levels independently of preoperative HbA1c. Peak 48-hour glucose levels were not included in the preoperative HbA1c model. All analyses were completed using SAS, version 9.4 (SAS Institute). Smoothed plots were developed using the R package GGPLOT2.20 Interaction terms were tested in the final model and included in the final model if statistically significant at P < .05.
Results
Patient and Procedural Characteristics
Patient and procedural factors stratified by a preoperative diagnosis of diabetes by VASQIP are summarized in Table 1. The mean age for the overall cohort was 63.7 years. Most patients were men (n = 20 348, 94.5%). Patients with diabetes who were insulin-dependent had a higher BMI (32.0 vs 30.1; P < .001), included more patients with an ASA classification of 4 to 5 (19.8% vs 13.3%; P < .001), experienced more postoperative complications (29.8% vs 26.6%; P < .001), and had more 30-day readmissions (16.6% vs 14.2%; P < .001). Patients with diabetes who were insulin-dependent also had higher preoperative glucose levels (166.1 vs 133.4 mg/dL; P < .001), initial postoperative glucose levels (190.7 vs 160.0 mg/dL; P < .001), and peak 48-hour postoperative glucose levels (230.8 vs 182.0 mg/dL; P < .001). The mean HbA1c for the cohort was 6.7%, with 7.0% among patients with diabetes who were noninsulin-dependent and 8.0% among patients with diabetes who were insulin-dependent (P < .001). Of 10 545 patients who did not receive a preoperative diagnosis of diabetes, the mean HbA1c was 5.9%, with 3986 patients (37.8%) having 5.7% or less (normal), 5420 (51.4%) ranging from 5.7% to 6.4% (prediabetic), and 1139 (10.8%) more than 6.5%, diagnostic of diabetes.
Table 1. Patient Factors, Procedural Factors, and Outcomes by Diabetes Status.
| Characteristic | All (n = 21 541) |
Nondiabetic (n = 10 545, 49.0%) |
NIDDM (n = 5857, 27.2%) |
IDDM (n = 5139, 23.9%) |
P Value |
|---|---|---|---|---|---|
| Patient Factors | |||||
| Age, mean (SD), y | 63.7 (10.6) | 62.8 (11.6) | 65.1 (9.6) | 64.1 (9.4) | <.001 |
| Sex, No. (%) | |||||
| Women | 1193 (5.5) | 707 (6.7) | 293 (5.0) | 195 (3.8) | <.001 |
| Men | 20 348 (94.5) | 9838 (93.3) | 5564 (95.0) | 4944 (96.2) | |
| BMI, % | 30.1 (7.2) | 28.7 (6.9) | 31.0 (6.9) | 32.0 (7.5) | <.001 |
| ASA classification, No. (%) | |||||
| 1-2 | 2675 (12.4) | 1930 (18.3) | 492 (8.4) | 251 (4.9) | <.001 |
| 3 | 16 007 (74.3) | 7476 (70.9) | 4662 (79.6) | 3870 (75.3) | |
| 4-5 | 2855 (13.3) | 1139 (10.8) | 703 (12.0) | 1018 (19.8) | |
| Preoperative HbA1c | |||||
| Closest within 90 d, mean (SD) | 6.7 (1.5) | 5.9 (0.7) | 7.0 (1.3) | 8.0 (1.7) | <.001 |
| <5.7%, No. (%) | 4601 (21.4) | 3986 (37.8) | 416 (7.1) | 200 (3.9) | <.001 |
| 5.7-6.5%, No. (%) | 8118 (37.7) | 5420 (51.4) | 1968 (33.6) | 730 (14.2) | |
| >6.5%, No. (%) | 8822 (41.0) | 1139 (10.8) | 3479 (59.4) | 4209 (81.9) | |
| Glucose level, mean (SD), mg/dL | |||||
| Closest preoperative | 133.4 (52.8) | 111.7 (30.7) | 143.9 (50.1) | 166.1 (69.0) | <.001 |
| Closest postoperative | 160.0 (54.4) | 136.3 (39.8) | 171.0 (50.1) | 190.7 (62.3) | <.001 |
| Highest postoperative | 182.0 (69.1) | 146.4 (48.8) | 196.4 (60.8) | 230.8 (73.8) | <.001 |
| Procedural factors | |||||
| Emergency case, No. (%) | 2667 (12.4) | 1392 (13.2) | 627 (10.7) | 653 (12.7) | <.001 |
| Postoperative LOS, d | 6.3 (4.9) | 6.3 (4.9) | 6.2 (4.8) | 6.5 (5.0) | <.001 |
| Outcomes | |||||
| Any postoperative complication, No. (%) | 5731 (26.6) | 2657 (25.2) | 1540 (26.3) | 1531 (29.8) | <.001 |
| Infectious complications, No. (%) | |||||
| Wound infection | 1230 (5.7) | 559 (5.3) | 334 (5.7) | 339 (6.6) | .003 |
| Pneumonia | 274 (1.3) | 148 (1.4) | 64 (1.1) | 67 (1.3) | .26 |
| UTI | 448 (2.1) | 190 (1.8) | 129 (2.2) | 123 (2.4) | .03 |
| Sepsis | 412 (1.9) | 190 (1.8) | 105 (1.8) | 113 (2.2) | .33 |
| Postdischarge outcomes, No. (%) | |||||
| Readmission within 14 d | 2175 (10.1) | 981 (9.3) | 586 (10.0) | 606 (11.8) | <.001 |
| Readmission within 30 d | 3048 (14.2) | 1371 (13.0) | 820 (14.0) | 853 (16.6) | <.001 |
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HbA1c, hemoglobin A1c; IDDM, insulin-dependent diabetes mellitus; LOS, length of stay; NIDDM, noninsulin dependent diabetes mellitus; UTI, urinary tract infection.
To convert to millimoles per liter, multiply by 0.0555.
To convert to the proportion of total hemoglobin, multiply by 0.01.
Postoperative Complications by HbA1c and Glucose
Elevated preoperative HbA1c was associated with decreased postoperative complications even after adjusting for age, sex, ASA class, wound class, work relative value units, postoperative hospital length of stay, diabetes diagnosis, and insulin use (Table 2). As compared with patients with normal HbA1c (<5.7%), patients with HbA1c more than 6.5% were significantly less likely to develop any postoperative complications (odds ratio [OR], 0.89; 95% CI, 0.80-0.99; P = .03) or to be readmitted within 30 days (OR, 0.85; 95% CI, 0.74-0.96; P = .01). The frequencies of each complication stratified by preoperative HbA1c are summarized in Table 3.
Table 2. Unadjusted and Adjusted ORs of Postoperative Complication by Preoperative Hemoglobin A1c and Postoperative Blood Glucose Levelsa.
| Outcome | Preoperative HbA1c %, OR (95% CI) | Peak 48-h Postoperative Blood Glucose Level, mg/dL, OR (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| Normal (<5.7%) |
Prediabetic (5.7%-6.4%) |
Diabetic (>6.5%) |
<120 | 120-180 | 180-250 | >250 | |
| Unadjusted | |||||||
| Any postoperative complication | 1 [Reference] | 0.93 (0.86-1.02) | 1.03 (0.95-1.11) | 1 [Reference] | 1.28 (1.15-1.42) | 1.41 (1.26-1.58) | 1.60 (1.41-1.82) |
| All infectious complications | |||||||
| Wound infection | 1 [Reference] | 0.89 (0.76-1.05) | 0.94 (0.79-1.11) | 1 [Reference] | 1.32 (1.06-1.62) | 1.53 (1.22-1.91) | 1.48 (1.15-1.90) |
| Pneumonia | 1 [Reference] | 0.94 (0.69-1.29) | 0.59 (0.42-0.84) | 1 [Reference] | 1.67 (1.07-2.61) | 1.80 (1.11-2.89) | 2.17 (1.27-3.70) |
| UTI | 1 [Reference] | 0.95 (0.73-1.25) | 0.94 (0.71-1.24) | 1 [Reference] | 1.59 (1.09-2.31) | 2.15 (1.46-3.17) | 2.21 (1.44-3.40) |
| Sepsis | 1 [Reference] | 0.95 (0.72-1.25) | 0.83 (0.62-1.11) | 1 [Reference] | 1.86 (1.25-2.78) | 2.16 (1.42-3.29) | 2.80 (1.77-4.40) |
| Postdischarge outcomes | |||||||
| Readmission within 14 d | 1 [Reference] | 0.99 (0.87-1.12) | 0.92 (0.81-1.06) | 1 [Reference] | 1.11 (0.95-1.30) | 1.28 (1.09-1.52) | 1.54 (1.28-1.86) |
| Readmission within 30 d | 1 [Reference] | 0.95 (0.85-1.06) | 0.86 (0.77-0.97) | 1 [Reference] | 1.16 (1.01-1.32) | 1.28 (1.11-1.48) | 1.63 (1.39-1.91) |
| Adjusted | |||||||
| Any postoperative complication | 1 [Reference] | 0.95 (0.87-1.04) | 0.89 (0.80-1.00) | 1 [Reference] | 1.04 (0.93-1.16) | 1.03 (0.90-1.17) | 1.12 (0.97-1.29) |
| All infectious complications | |||||||
| Wound infection | 1 [Reference] | 0.91 (0.77-1.09) | 0.95 (0.78-1.17) | 1 [Reference] | 1.01 (0.82-1.26) | 1.04 (0.82-1.33) | 0.99 (0.75-1.30) |
| Pneumonia | 1 [Reference] | 1.04 (0.75-1.45) | 0.77 (0.51-1.17) | 1 [Reference] | 0.95 (0.60-1.51) | 0.81 (0.48-1.36) | 0.82 (0.46-1.47) |
| UTI | 1 [Reference] | 0.93 (0.70-1.23) | 0.98 (0.70-1.35) | 1 [Reference] | 0.99 (0.67-1.46) | 1.07 (0.70-1.62) | 1.03 (0.64-1.64) |
| Sepsis | 1 [Reference] | 1.04 (0.78-1.39) | 1.02 (0.72-1.44) | 1 [Reference] | 1.09 (0.72-1.66) | 1.02 (0.65-1.61) | 1.22 (0.74-2.00) |
| Postdischarge outcomes | |||||||
| Readmission within 14 d | 1 [Reference] | 1.01 (0.88-1.15) | 0.89 (0.76-1.05) | 1 [Reference] | 0.98 (0.83-1.15) | 1.04 (0.86-1.24) | 1.19 (0.97-1.46) |
| Readmission within 30 d | 1 [Reference] | 0.96 (0.85-1.07) | 0.81 (0.71-0.93) | 1 [Reference] | 0.99 (0.86-1.14) | 0.98 (0.84-1.15) | 1.18 (0.99-1.41) |
Abbreviations: HbA1c, hemoglobin A1c; OR, odds ratio; UTI, urinary tract infection.
To convert to millimoles per liter, multiply by 0.0555.
To convert to the proportion of total hemoglobin, multiply by 0.01.
Adjusted for sex, age, body mass index (calculated as weight in kilograms divided by height in meters squared), American Society of Anesthesiologists classification, wound classification, work relative value unit, postoperative hospital length of stay, preoperative diabetes, and postoperative insulin use.
Table 3. Complications by Preoperative Hemobglobin A1c.
| No. (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Preoperative HbA1c, % | Peak 48-h Postoperative Glucose Level, mg/dL | ||||||||
| Normal (<5.7) |
Prediabetic (5.7-6.4) |
Diabetic (≥6.5) |
P Value | <120 | 120-180 | 180-250 | >250 | P Value | |
| Any postoperative complication | 1346 (27.3) | 2248 (26.1) | 2683 (28.1) | .01 | 2084 (26.5) | 1614 (28.1) | 571 (22.2) | 1094 (30.2) | <.001 |
| Infectious complications | |||||||||
| Wound infection | 270 (5.5) | 445 (5.2) | 594 (6.2) | .01 | 452 (5.7) | 381 (6.6) | 114 (4.4) | 232 (6.4) | <.001 |
| Pneumonia | 76 (1.5) | 125 (1.5) | 104 (1.1) | .03 | 114 (1.5) | 76 (1.3) | 24 (0.9) | 49 (1.4) | .26 |
| UTI | 89 (1.8) | 173 (2.0) | 220 (2.3) | .11 | 159 (2.0) | 145 (2.5) | 34 (1.3) | 87 (2.4) | .003 |
| Sepsis | 95 (1.9) | 171 (2.0) | 199 (2.1) | .80 | 157 (2.0) | 121 (2.1) | 29 (1.1) | 89 (2.5) | .003 |
| Postdischarge outcomes | |||||||||
| Readmission within 14 d | 494 (10.0) | 867 (10.1) | 1038 (10.9) | .13 | 756 (9.6) | 617 (10.7) | 227 (8.8) | 447 (12.3) | <.001 |
| Readmission within 30 d | 716 (14.5) | 1222 (14.2) | 1453 (15.2) | .13 | 1083 (13.8) | 842 (14.6) | 316 (12.3) | 633 (17.5) | <.001 |
Abbreviations: HbA1c, hemoglobin A1c; UTI, urinary tract infection.
By contrast, elevated peak 48-hour postoperative blood glucose levels were associated with increased odds for developing postoperative complications, but these associations were only marginally significant after adjusting for other patient characteristics (Table 2). After adjustment, only 30-day readmissions remained significantly associated with peak 48-hour postoperative glucose levels (>250 vs <120 mg/dL; OR, 1.20; 95% CI, 1.01-1.42).
The interaction of preoperative HbA1c and postoperative glucose was of specific interest, but we failed to find a statistically significant interaction between the 2 terms in the adjusted model, and it was therefore not included in the final model.
Postoperative Glucose Level Surveillance
The mean total glucose level was 4.92 for patients with an HbA1c of less than 5.7%, 6.89 for patients with an HbA1c ranging from 5.7% to 6.4%, and 9.71 for patients with an HbA1c of more than 6.5% (P < .001). The frequency of hyperglycemia surveillance by means of glucose level checks increased as the preoperative HbA1c increased from 3% to 10% (Figure 2A).
Figure 2. Postoperative Glucose Level Surveillance and Hyperglycemic Treatment.
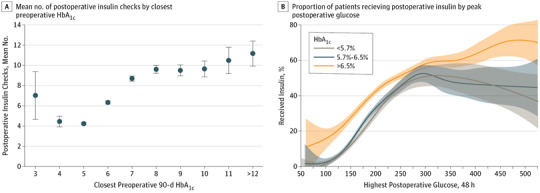
A, Mean number of postoperative insulin checks by closest preoperative hemoglobin AIc (HbA1c). Error bar represents mean 95% CI. B, Proportion of patients receiving postoperative insulin by peak postoperative glucose level. The gray shaded area represents glucose levels less than 5.7%
Postoperative Hyperglycemia Treatment
Patients with preoperative HbA1c more than 6.5% have lower thresholds for insulin use per postoperative glucose until their glucose level reaches 240 mg/dL, in which insulin use equalizes across all preoperative HbA1c categories (Figure 2B). The closest preoperative HbA1c and glucose levels, as well as the highest 48-hour glucose levels, were the strongest predictors of receiving insulin in the 48 hours following surgery. Overall, patients with an HbA1c ranging from 5.7% to 6.4% were not more likely to receive insulin compared with patients with an HbA1c of less than 5.7%. However, patients with an HbA1c of more than 6.5% were 1 to 3 times more likely to receive insulin when their postoperative glucose values were less than 250 mg/dL. Specifically, 530 patients (11.5%) with an HbA1c of 5.7% or less received insulin compared with 1422 (17.5%) with an HbA1c ranging from 5.7% to 6.4% and 3895 (44.2%) with an HbA1c of more than 6.4 (P < .01). Once the postoperative glucose level reaches 250 mg/dL, all patients have an equal opportunity to receive insulin regardless of postoperative glucose levels. Other factors associated with insulin use are age, sex, BMI, ASA classification, preoperative diabetes, preoperative sepsis, and hypertensive medications.
Discussion
Patients with insulin-dependent diabetes have higher postoperative complication rates compared with patients with noninsulin-dependent diabetes and those without diabetes.4,5 They also have higher 14- and 30-day readmission rates. Even after adjusting for diabetes, preoperative HbA1c, insulin use, and BMI, patients with peak 48-hour postoperative blood glucose levels of more than 250 mg/dL are 20% more likely to be readmitted within 30 days. Contrary to this, patients with a preoperative HbA1c of more than 6.5% are 17% less likely to be readmitted within 30 days. We hypothesized that because HbA1c is known preoperatively, hyperglycemia in these patients is more vigilantly monitored and treated with insulin. Our findings indicated that the frequency of glucose level checks increased with increasing HbA1c until HbA1c equals 10%. In addition, the threshold to treat hyperglycemia with insulin was lower for patients with an HbA1c of more than 6.5%.
The association between postoperative hyperglycemia and infectious complications is consistent with prior findings.8,10 We believe that postoperative hyperglycemia reflects an acute inflammatory phase and the host’s response that may lead to increased postoperative complications. Kotagel et al21 described a dose-dependent association between hyperglycemia and adverse events among patients without diabetes. The authors attributed this finding to several theories, including that patients with diabetes may be more likely to be tested and treated for hyperglycemia. Our findings suggest this theory holds true, and our study expands on this work by looking at readmissions.
The current literature lacks consensus regarding the association between HbA1c and postoperative complications that lead to readmission,12,22 and the finding of elevated HbA1c as protective of postoperative complications and readmissions is novel. It has been proposed that HbA1c is the most significant predictor of postoperative complications, partially because preoperative hyperglycemia corresponds to postoperative hyperglycemia and the ability to control it.17 As opposed to creating separate models for preoperative and postoperative hyperglycemia, we created one model that accounted for HbA1c, postoperative hyperglycemia, diabetes status, and insulin use and found that HbA1c was not a significant predictor of complications and was protective of 30-day readmission.
We tested whether elevated HbA1c is protective of postoperative complications and thereby readmissions because of the increased monitoring and treatment of hyperglycemia in these patients. Only 59% of hospitalized patients undergo glucose monitoring and, of these that are found to be hyperglycemic, only 54% are treated with insulin.23 Because the risk of postoperative complications corresponds to the degree of hyperglycemia experienced, many have advocated for increased glycemic monitoring and consideration for early management.24 However, it has been demonstrated that patients without diabetes are less likely to receive insulin for hyperglycemia.25 As patients with elevated HbA1c are considered to have poorly controlled diabetes, we observed that their postoperative course is marked by vigilant glycemic monitoring and intervention that may explain the observation of improved outcomes compared with patients with normal HbA1c. While many advocate for deferring elective surgery in patients with elevated HbA1c until it is optimized,17 our results suggest that proceeding may be acceptable as long as there is vigilant postoperative glucose level monitoring and treatment.
Strengths and Limitations
Our study was limited to patients undergoing gastrointestinal surgery, among whom there are studies on the relationship of diabetes and hyperglycemia on postoperative outcomes. A strength of this study is the use of all glucose measurements and treatment in a national cohort of patients undergoing surgery to evaluate the association of perioperative glucose on complications and readmissions. However, it also has its limitations. We chose to categorize HbA1c based on the American Diabetes Association cutoffs for normal (<5.7%), prediabetes (5.7 – 6.4%), and diabetes (>6.5%). This study does not delineate the outcomes for elevated HbA1c of more than 7%, more than 8%, or even more than 10%, in which the power is lacking. In addition, because we excluded patients who died in the hospital to examine readmissions, patients with the most severe complications resulting in in-hospital death were excluded from this study. However, since we hypothesized that postoperative hyperglycemia was associated with worse outcomes, this limitation would result in bias toward the null. While all patients underwent a procedure in the general surgery specialty, they did not undergo the same procedure. Because we did not compare the specific type of surgery and patient perioperative glucose or HbA1c, it is possible that the results were affected. In addition, there are several potential confounders, including laparoscopic vs open procedure, indications for surgery, and antibiotic use, which were not addressed and could limit the study. We also excluded patients without preoperative HbA1c within 90 days of undergoing surgery or a postoperative glucose level assessment, which may have introduced selection bias (eTable 1 in the Supplement). Finally, because our data source is the VA, our patient population is predominantly male and as a retrospective study, we cannot assess causation.
Conclusions
In summary, early postoperative glucose increases the risk of 30-day readmission, whereas elevated preoperative HbA1c is associated with decreased readmission potentially because of more intensive monitoring and intervention of postoperative hyperglycemia. These findings advocate for increased glycemic monitoring in the early postoperative phase and early treatment of hyperglycemia to maintain peak blood glucose levels of less than 250 mg/dL to minimize the risk for complications because of hyperglycemia. Further study is warranted to address causation.
eTable. Characteristics of Patients Missing Preoperative HbA1c or Preoperative Glucose.
References
- 1.Buehler L, Fayfman M, Alexopoulos AS, et al. The impact of hyperglycemia and obesity on hospitalization costs and clinical outcome in general surgery patients. J Diabetes Complications. 2015;29(8):1177-1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sacks DB, John WG. Interpretation of hemoglobin A1c values. JAMA. 2014;311(22):2271-2272. [DOI] [PubMed] [Google Scholar]
- 3.Chamberlain JJ, Rhinehart AS, Shaefer CF Jr, Neuman A. Diagnosis and management of diabetes: synopsis of the 2016 American Diabetes Association Standards of Medical Care in Diabetes. Ann Intern Med. 2016;164(8):542-552. [DOI] [PubMed] [Google Scholar]
- 4.Dronge AS, Perkal MF, Kancir S, Concato J, Aslan M, Rosenthal RA. Long-term glycemic control and postoperative infectious complications. Arch Surg. 2006;141(4):375-380. [DOI] [PubMed] [Google Scholar]
- 5.Underwood P, Askari R, Hurwitz S, Chamarthi B, Garg R. Preoperative A1C and clinical outcomes in patients with diabetes undergoing major noncardiac surgical procedures. Diabetes Care. 2014;37(3):611-616. [DOI] [PubMed] [Google Scholar]
- 6.Moitra VK, Greenberg J, Arunajadai S, Sweitzer B. The relationship between glycosylated hemoglobin and perioperative glucose control in patients with diabetes. Can J Anaesth. 2010;57(4):322-329. [DOI] [PubMed] [Google Scholar]
- 7.Ito N, Iwaya T, Ikeda K, et al. Hyperglycemia 3 days after esophageal cancer surgery is associated with an increased risk of postoperative infection. J Gastrointest Surg. 2014;18(9):1547-1556. [DOI] [PubMed] [Google Scholar]
- 8.Frisch A, Chandra P, Smiley D, et al. Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care. 2010;33(8):1783-1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richards JE, Hutchinson J, Mukherjee K, et al. Stress hyperglycemia and surgical site infection in stable nondiabetic adults with orthopedic injuries. J Trauma Acute Care Surg. 2014;76(4):1070-1075. [DOI] [PubMed] [Google Scholar]
- 10.Ramos M, Khalpey Z, Lipsitz S, et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg. 2008;248(4):585-591. [DOI] [PubMed] [Google Scholar]
- 11.Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D. Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg. 2013;257(1):8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.King JT Jr, Goulet JL, Perkal MF, Rosenthal RA. Glycemic control and infections in patients with diabetes undergoing noncardiac surgery. Ann Surg. 2011;253(1):158-165. [DOI] [PubMed] [Google Scholar]
- 13.Noordzij PG, Boersma E, Schreiner F, et al. Increased preoperative glucose levels are associated with perioperative mortality in patients undergoing noncardiac, nonvascular surgery. Eur J Endocrinol. 2007;156(1):137-142. [DOI] [PubMed] [Google Scholar]
- 14.Lee LJ, Emons MF, Martin SA, et al. Association of blood glucose levels with in-hospital mortality and 30-day readmission in patients undergoing invasive cardiovascular surgery. Curr Med Res Opin. 2012;28(10):1657-1665. [DOI] [PubMed] [Google Scholar]
- 15.Ata A, Lee J, Bestle SL, Desemone J, Stain SC. Postoperative hyperglycemia and surgical site infection in general surgery patients. Arch Surg. 2010;145(9):858-864. [DOI] [PubMed] [Google Scholar]
- 16.Hwang JS, Kim SJ, Bamne AB, Na YG, Kim TK. Do glycemic markers predict occurrence of complications after total knee arthroplasty in patients with diabetes? Clin Orthop Relat Res. 2015;473(5):1726-1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goodenough CJ, Liang MK, Nguyen MT, et al. Preoperative glycosylated hemoglobin and postoperative glucose together predict major complications after abdominal surgery. J Am Coll Surg. 2015;221(4):854-861.e1. [DOI] [PubMed] [Google Scholar]
- 18.Davis CL, Pierce JR, Henderson W, et al. Assessment of the reliability of data collected for the Department of Veterans Affairs national surgical quality improvement program. J Am Coll Surg. 2007;204(4):550-560. [DOI] [PubMed] [Google Scholar]
- 19.Morris MS, Graham LA, Richman JS, et al. Postoperative 30-day readmission: time to focus on what happens outside the hospital. Ann Surg. 2016;264(4):621-631. [DOI] [PubMed] [Google Scholar]
- 20.Wickham H. GGPLOT2: Elegant Graphics for Data Analysis. New York, NY: Springer; 2009. [Google Scholar]
- 21.Kotagal M, Symons RG, Hirsch IB, et al. ; SCOAP-CERTAIN Collaborative . Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg. 2015;261(1):97-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Engoren M, Schwann TA, Habib RH. Elevated hemoglobin A1c is associated with readmission but not complications. Asian Cardiovasc Thorac Ann. 2014;22(7):800-806. [DOI] [PubMed] [Google Scholar]
- 23.Levetan CS, Passaro M, Jablonski K, Kass M, Ratner RE. Unrecognized diabetes among hospitalized patients. Diabetes Care. 1998;21(2):246-249. [DOI] [PubMed] [Google Scholar]
- 24.Kiran RP, Turina M, Hammel J, Fazio V. The clinical significance of an elevated postoperative glucose value in nondiabetic patients after colorectal surgery: evidence for the need for tight glucose control? Ann Surg. 2013;258(4):599-604. [DOI] [PubMed] [Google Scholar]
- 25.Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978-982. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Characteristics of Patients Missing Preoperative HbA1c or Preoperative Glucose.


