Abstract
Polyubiquitination of proteins has a pivotal role in the regulation of numerous cellular functions such as protein degradation, DNA repair and cell signaling. As deregulation of these processes can result in pathological conditions such as inflammatory diseases, neurodegeneration or cancer, tight regulation of the ubiquitin system is of tremendous importance. Ubiquitination by E3 ubiquitin ligases can be counteracted by the activity of several deubiquitinating enzymes (DUBs). CYLD, A20 and OTULIN have been implicated as key DUBs in the negative regulation of NF-κB transcription factor-mediated gene expression upon stimulation of cytokine receptors, antigen receptors and pattern recognition receptors, by removing distinct types of polyubiquitin chains from specific NF-κB signaling proteins. In addition, they control TNF-induced cell death signaling leading to apoptosis and necroptosis via similar mechanisms. In the case of A20, also catalytic-independent mechanisms of action have been demonstrated to have an important role. CYLD, A20 and OTULIN have largely overlapping substrates, suggesting at least partially redundant functions. However, mice deficient in one of the three DUBs show significant phenotypic differences, indicating also non-redundant functions. Here we discuss the activity and polyubiquitin chain-type specificity of CYLD, A20 and OTULIN, their specific role in NF-κB signaling and cell death, the molecular mechanisms that regulate their activity, their role in immune homeostasis and the association of defects in their activity with inflammation, autoimmunity and cancer.
Similar content being viewed by others
Facts
-
CYLD, A20 and OTULIN are key DUBs in the regulation of NF-κB and cell death signaling.
-
CYLD, A20 and OTULIN target partially overlapping protein substrates.
-
CYLD, A20 and OTULIN hydrolyze M1 and K63 polyubiquitin chains with different specificities.
-
A20 has catalytic-independent mechanisms of action.
-
Defects in CYLD, A20 or OTULIN are associated with inflammation, autoimmunity and cancer.
Open Questions
-
Why are (at least) three different DUBs with partially overlapping activities required to regulate NF-κB signaling and cell death?
-
How is the catalytic activity or substrate binding capacity turned on or off?
-
Do CYLD and OTULIN have catalytic-independent activities similar to A20?
-
Is there crosstalk between the different DUBs?
-
Can we modulate CYLD, A20 and OTULIN activity for therapeutic purposes?
The Ubiquitination/Deubiquitination Machinery
Ubiquitination has emerged as one of the most important post-translational modifications in various cellular processes by regulating protein degradation, autophagy, intracellular protein trafficking, DNA damage responses, protein activation and protein–protein interactions.1 This diversity of functions is achieved by the ability to form eight structurally different types of polyubiquitin chains where the C-terminal glycine of the distal ubiquitin molecule is attached to one of the seven lysine residues (K6, K11, K27, K29, K33, K48 and K63) or the N-terminal methionine (M1) within the proximal ubiquitin residue. Things got even more complex with the identification of mixed chain types such as M1/K63 and K48/K63 hybrid chains.2, 3 K48 polyubiquitination mainly marks proteins for proteasomal degradation, whereas K63 and M1 polyubiquitin chains are non-degradative and serve as important regulators of immune-related signaling. Different types of ubiquitination are recognized by specific ubiquitin-binding domain (UBD)-containing proteins that mediate downstream signaling. Ubiquitination can be reversed by deubiquitinating enzymes (DUBs). Human cells contain ~100 DUBs belonging to six families. Five families, the ovarian tumor (OTU), the ubiquitin-specific proteases (USPs), the ubiquitin C-terminal hydrolases, the Josephin domain family and the newly discovered motif interacting with ubiquitin-containing novel DUB family (MINDY) are papain-like cysteine proteases, whereas JAB1/MPN/Mov34 metalloenzyme domain family members are zinc-dependent metalloproteases.4, 5 Mutations in specific DUBs have been linked with neurodegeneration, chronic inflammation, autoimmunity, infectious disease and cancer. Several DUBs, such as CYLD, A20 and OTULIN, act as negative regulators of NF-κB signaling and have an important role in TNF-induced cell death signaling.
CYLD
Activity and specificity of CYLD
The N-terminal part of CYLD comprises three cytoskeleton-associated protein-glycine-rich (CAP-Gly) domains (Figure 1), the first two mediating microtubule binding, whereas the third CAP-Gly domain binds to the inhibitor of κB (IκB) kinase (IKK) adaptor protein NEMO.6, 7 CYLD further contains two conserved proline-rich (PR) motifs, which may interact with SH3 domains in other proteins, and a TRAF2-binding motif (PVQES). The C-terminal part of CYLD contains a catalytic USP domain that mediates the cleavage of various polyubiquitin linkages with a preference for K63 and M1 polyubiquitin, and to a lesser extent K11 and K48 polyubiquitin in vitro.8 Structural studies of the CYLD USP domain shed further light on how specificity for K63 and M1 polyubiquitin chains is achieved.9, 10, 11
Domain structure of CYLD, A20 and OTULIN. CYLD contains three cytoskeleton-associated protein glycine-rich (CAP-Gly) domains that mediate microtubule binding, two proline-rich (PR) motifs and the USP domain harboring its DUB activity. A20 consists of an OTU responsible for its DUB activity and seven C-terminal zinc finger (ZF) domains. ZF4 mediates E3 ligase activity as well as binding to K63 polyubiquitin. ZF7 specifically binds M1 polyubiquitin. OTULIN is mostly made up of its OTU domain. An N-terminal PUB-interacting motif (PIM) is essential for its interaction with HOIP. Catalytic cysteines conferring the DUB activity are indicated by a star. Proteolytic processing sites by caspase-8 and MALT1, as well as specific phosphorylation sites (P), are indicated. Amino-acid numbering is for the human proteins
CYLD in NF-κB signaling and cell death
CYLD has been extensively studied in the context of NF-κB signaling.6 In basal conditions NF-κB is sequestered in the cytosol by IκB proteins. In the classical NF-κB pathway, which is activated by a wide range of triggers, including TNFR, IL-1R, TLR and T- or B-cell receptor stimulation, receptor engagement activates the IKK complex, consisting of the catalytic subunits IKKα and IKKβ and the regulatory subunit NEMO (Figure 2). IKKβ phosphorylates IκBα, triggering its ubiquitination and degradation, thus allowing NF-κB translocation into the nucleus. CYLD removes K63 and M1 polyubiquitin chains from a range of NF-κB signaling proteins (Table 1 and Figure 2). Most recently, K48–K63 branching was shown to protect K63 linkages from CYLD-mediated deubiquitination.3 In agreement with its role in deubiquitinating several key NF-κB signaling proteins, CYLD deficiency leads to constitutive NF-κB activation resulting in proinflammatory gene expression.12, 13, 14
General principles of regulation of NF-κB signaling downstream of different receptors by CYLD, A20 and OTULIN. (Left) Toll-like receptor (TLR) or interleukin-1 receptor (IL-1R) stimulation leads to the recruitment of the adaptor protein MyD88 and the kinases IRAK1 and IRAK4. Subsequent recruitment of the E3 ligase TRAF6 results in the K63 poly ubiquitination of IRAK1/4 and TRAF6 itself. (Middle) T-cell receptor (TCR) or B-cell receptor (BCR) crosslinking by antigen results in the downstream activation of protein kinase C (PKC), which phosphorylates CARMA1, leading to the formation and activation of the CBM complex consisting of CARMA1, Bcl10 and MALT1. Recruitment of the E3 ligase TRAF6 to MALT1 leads to the modification of several signaling proteins with K63 polyubiquitin. (Right) TNF induces binding of TNFR1 to the adapter protein TRADD, which in turn recruits the kinase RIPK1 as well as the E3 ligases TRAF2 and TRAF5. TRAF2 interacts with the E3 ligases cIAP1 and cIAP2, which modify various TNFR1 complex components with K63 polyubiquitin. These serve for the recruitment of the linear ubiquitin assembly complex (LUBAC), which mediates the modification of TNFR1, TRADD, RIPK1 and NEMO with M1-linked chains, including the formation of mixed K63/M1 ubiquitin chains. (Bottom left) Following ligand sensing NOD2 binds RIPK2, which recruits cIAP family members (XIAP, cIAP1/2) that facilitate RIPK2 K63 poly ubiquitination, serving as a platform for LUBAC and the generation of M1 polyubiquitin. In all cases, ubiquitination serves to recruit and stabilize TAB2/TAB3/TAK1 and NEMO/IKK kinase complexes, leading to downstream activation of MAPKs (not shown) and NF-κB. NF-κB signaling is counteracted by the DUBs CYLD, A20 and OTULIN. CYLD and A20 remove K63 polyubiquitin from several substrates. In the case of TNFR1 signaling, A20-mediated K63 deubiquitination of RIPK1 is followed by its A20-mediated K48 ubiquitination (not shown), either directly or indirectly, resulting in its proteasomal degradation. Furthermore, binding of A20 to M1 polyubiquitin can prevent deubiquitination by other DUBs as well as interfere with ubiquitin-mediated protein–protein interactions. OTULIN specifically removes M1 polyubiquitin from its substrates
Loss of CYLD inhibits apoptosis by promoting NF-κB activation and NF-κB-dependent expression of prosurvival genes (Figure 3).12, 13, 14 Additionally, an siRNA screen for regulators of necroptosis revealed CYLD as an essential mediator of necroptosis, a caspase-independent form of programmed cell death that depends on RIPK1 and RIPK3 kinases.15 Furthermore, CYLD is negatively regulated by caspase-8-mediated cleavage, and expression of an uncleavable CYLD mutant facilitates TNF-induced necroptosis.16 Also, cells expressing uncleavable CYLD show decreased RIPK1 ubiquitination and RIPK1–NEMO interaction, and hence a destabilization of TNFR complex I. Moquin et al.17 demonstrated that CYLD regulates RIPK1 ubiquitination not only at the TNFR1 complex but also at the necrosome and thereby facilitates RIPK1 kinase activation and necroptosis (Figure 3). CYLD is not only required for necroptosis induced by TNF but also in response to stimulation of several TLRs. More specifically, constitutive transcriptional downregulation of CYLD in macrophages from the wild-derived inbred MOLF/EiJ mouse strain renders cells less susceptible to TLR3- and TLR4-induced necroptosis, independent of autocrine TNF signaling, most likely due to increased RIPK1 ubiquitination.18 TRIF-dependent TLR3/TLR4 signaling also activates caspase-8-mediated CYLD cleavage to protect cells from autonecroptosis.19 Taken together, CYLD regulates cell death pathways on two levels: (a) by regulating prosurvival gene expression via NF-κB, and (b) by regulating the ubiquitination status of RIPK1 and its commitment for complex I or II.
General principles of regulation of TNF-induced cell death signaling by CYLD- and A20-mediated deubiquitination. TNF-induced formation of signaling complex I (RIPK1, cIAP1/2, TRADD and TRAF2/5) at the cell membrane leads to the ubiquitin-dependent activation of NF-κB and the NF-κB-dependent expression of antiapoptotic genes. Deubiquitination of RIPK1 by CYLD inhibits NF-κB signaling, and leads to the formation of complex IIa (RIPK1, TRADD, caspase-8 and FADD) in the cytosol. Activation of caspase-8 in this complex results in apoptosis, and also the caspase-8-mediated cleavage of CYLD, restoring NF-κB signaling and imposing a delicate cell survival/apoptosis balance. In the presence of RIPK3, inhibition of caspases induces the formation of complex IIb (RIPK1/RIPK3/MLKL; also known as the necrosome) and the induction of necroptosis. Increased RIPK1 K63 ubiquitination in the necrosome correlates with impaired RIPK1 and RIPK3 phosphorylation and function. CYLD-mediated deubiquitination of RIPK1 in the necrosome facilitates necroptosis. A20 binding to M1 polyubiquitin protects them from degradation and stabilizes complex I. In addition, by binding to M1 chains, A20 also competes with ubiquitin-binding proteins like NEMO, thereby inhibiting downstream NF-κB activation. A20 also cleaves K63 polyubiquitin from RIPK3, thereby inhibiting RIPK1–RIPK3 interaction and necroptosis. The function of OTULIN in the regulation of cell death is less clear, as both, depletion and overexpression of OTULIN have been shown to sensitize to cell death
CYLD has a role in various other cellular processes including cell cycle progression, cell migration, DNA damage and Wnt signaling, which are extensively reviewed elsewhere.20, 21
Regulation of CYLD activity
CYLD is constitutively expressed in most cell types, but NF-κB-dependent transcriptional upregulation22 as well as miRNA-mediated downregulation of CYLD expression have been reported.23 At the protein level, CYLD is rapidly and transiently phosphorylated in response to TNF, LPS and mitogens on multiple residues within a serine cluster between amino acids 418 and 444.24 The presence of several IKKβ consensus phosphorylation sites in this cluster, the NEMO dependency of the inducible CYLD phosphorylation and the ability of recombinant IKKα and IKKβ to phosphorylate CYLD in vitro, is compatible with an important role for IKKs. Mechanistically, CYLD phosphorylation prevents CYLD-mediated TRAF2 deubiquitination and promotes TNF-induced gene expression.24 Another group showed that CYLD is phosphorylated at Ser418 upon coexpression of the IKKβ-related kinase IKKɛ, leading to decreased DUB activity and contributing to cellular transformation.25 IKKɛ-dependent Ser418 phosphorylation and inactivation of CYLD has also been reported in response to stimulation of the C-type lectin receptor DC-SIGN in dendritic cells, resulting in the accumulation and nuclear translocation of ubiquitinated Bcl3, which modulates cytokine expression.26 A contradictory report, showing that CYLD Ser418 phosphorylation increases its DUB activity towards K63 polyubiquitin in vitro,27 illustrates that the molecular mechanisms and biological function of CYLD phosphorylation are far from clear.
As mentioned above, CYLD can be inactivated by caspase-8-mediated cleavage at Asp215 in response to TNF and TLR stimulation.16, 19 Our group showed that paracaspase MALT1 cleaves CYLD upon TCR stimulation at Arg324, separating the N-terminal first two CAP-Gly domains from the third CAP-Gly domain and the C-terminal catalytic domain.28 MALT1-mediated CYLD cleavage promotes TCR-induced JNK activation and gene expression, but does not affect NF-κB activation. MALT1-dependent CYLD cleavage also has a role in the initiation of T-cell acute lymphoblastic leukemia (T-ALL).29 More specifically, ectopic expression of the N-terminal CYLD cleavage fragment is sufficient to transform human PBMCs into cells with a T-ALL-like phenotype. Recently, thrombin-induced MALT1-mediated CYLD cleavage was shown to interfere with its microtubule-destabilizing function, leading to endothelial cell retraction and disruption of the endothelial barrier integrity.30
CYLD is ubiquitinated by SCFβ-TRCP in response to RANK triggering, leading to its proteasomal degradation and accumulation of ubiquitinated TRAF6, which contributes to RANKL-induced osteoclastogenesis.31 CYLD ubiquitination is dependent on prior phosphorylation at Ser432/436 by IKKβ. Additionally, in neuroblastoma cells it has been reported that CYLD activity can be directly inhibited by SUMOylation.32
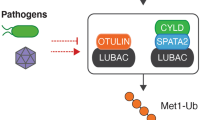
CYLD physically interacts with several UBD-containing proteins as well as E3 ubiquitin ligases, adding another level of fine-tuning to CYLD activity. In particular, CYLD physically interacts with ubiquitin adapters p62 and OPTN to approach its substrates TRAF6 and RIPK1 in RANKL- and TNF-induced NF-κB signaling, respectively.33, 34 CYLD also interacts with the E3 ubiquitin ligase Itch to sequentially remove K63 polyubiquitin from and add K48 polyubiquitin to the kinase TAK1, thus regulating inflammatory signaling.35 Furthermore, CYLD associates with the E3 ubiquitin ligase HOIP,36 which is the catalytic subunit of the linear ubiquitin chain assembly complex (LUBAC). Recently, several reports demonstrated that this interaction is facilitated by SPATA2.37, 38, 39, 40 More specifically, the N-terminal PNGase/UBA or UBX (PUB) domain of SPATA2 interacts with the USP domain of CYLD, whereas the C-terminal PUB-interacting motif (PIM) of SPATA2 interacts with the HOIP PUB domain.37, 38, 39 SPATA2 already binds to CYLD and LUBAC under steady-state conditions and mediates CYLD recruitment to TNFR1 and NOD2 signaling complexes in stimulated cells.37, 38, 39, 40 Binding of SPATA2 to CYLD also activates its DUB activity,37, 39 resulting in CYLD-mediated removal of M1 and K63 polyubiquitin from specific substrates in TNFR1 (RIPK1, TNFR1 and TRADD) and NOD2 (RIPK2) signaling complexes.41, 42 In agreement, SPATA2 deficiency increases TNF-induced NF-κB activation and decreases TNF-induced necroptosis.38, 39, 40
CYLD in tissue homeostasis and disease
CYLD was originally identified as a tumor suppressor gene mutated in familial cylindromatosis, a genetic condition that predisposes patients to develop multiple neoplasms of skin appendages.12, 14, 43 More recently, a tumor suppressor function for CYLD has been described in other cancers, with the majority of CYLD mutations and truncations found in patients negatively affecting its expression or DUB activity.44 Genome-wide association studies revealed that CYLD polymorphisms are associated with inflammatory bowel disease.45
Various CYLD genetic mouse models illustrate the important regulatory function of CYLD in diverse biological processes, including immune cell development and function, innate immunity, osteoclastogenesis, spermatogenesis and hepatocellular homeostasis. Table 3 gives an overview of the different CYLD knockout and knock-in mouse models and their phenotypes. Of note, different conclusions regarding cell-type-specific roles of CYLD were made in studies using independently generated CYLD-deficient mice, which may be due to compensatory mechanisms by redundant proteins, or dominant-negative functions of truncated CYLD.
A20
Activity and specificity of A20
A20, also known as TNFAIP3 (TNFα-induced protein 3), contains an N-terminal OTU domain, whereas the C-terminal part contains seven Cys2-Cys2 zinc-finger (ZF) domains (Figure 1).46 While A20 hydrolyzes K48 and K11 polyubiquitin and to a lesser extent K63 polyubiquitin in vitro,46, 47 it exhibits strong activity towards K63-polyubiquitinated substrates in cells.48, 49 In agreement, IKKβ-mediated A20 phosphorylation at Ser381 increases A20s in vitro DUB activity towards K63 polyubiquitin, indicating a role for post-translational modifications in the regulation of A20 activity.50 Next to its DUB activity, A20 was originally shown to hold E3 ubiquitin ligase activity that is mediated by its ZF4, enabling a dual ubiquitin-editing function. More specifically, A20 replaces K63 polyubiquitin from RIPK1 with K48 polyubiquitin, leading to its proteasomal degradation.49 Although in vitro studies with recombinant A20 showed a direct E3 ubiquitin ligase activity,49 in cells A20-associated E3 ubiquitin ligases such as RNF11 and Itch may be involved in A20-mediated K48 ubiquitination.51, 52 Finally, A20 ZFs act as ubiquitin-binding domains: A20 ZF4 binds K63 polyubiquitin,53 whereas ZF7 binds M1 polyubiquitin.54, 55
A20 in NF-κB signaling and cell death
Similar to CYLD, A20 is an important regulator of inflammatory signaling and cell death. A20 is an NF-κB-responsive gene that is involved in the negative feedback regulation of NF-κB activation in response to many proinflammatory stimuli including TNF, IL-1, LPS, T- and B-cell receptor antigens, and NOD2 ligands (Figure 2).56 A20 DUB activity disassembles K63 polyubiquitin from multiple NF-κB signaling intermediates (Table 1), which has been proposed to mediate its NF-κB inhibitory function. In addition, A20 mediates K48 ubiquitination of several substrates (Table 2), leading to their degradation and subsequent inhibition of downstream signaling. Despite numerous reports describing a role for A20 DUB activity in the regulation of NF-κB signaling, the physiological relevance of A20 catalytic activity has recently been challenged by the finding that A20 knock-in mice bearing an inactivating mutation in DUB or ZF4 domains do not mimic the severe inflammatory phenotype of full A20-knockout mice.57, 58, 59 Furthermore, reconstitution of A20-deficient MEF cells with the corresponding mutant proteins does not or only marginally abolishes A20 ability to inhibit TNF-induced NF-κB activation,58, 59, 60 suggesting a non-catalytic mechanism of action. Indeed, multiple examples illustrate the ability of A20 to modulate ubiquitin-dependent signaling via non-catalytic mechanisms (Table 2). Binding of A20 to K63 and M1 polyubiquitin via its ZF4 and ZF7, respectively, recruits A20 to ubiquitinated proteins at the TNFR1 signaling complex, where it may compete with other ubiquitin-binding proteins such as NEMO to prevent IKK activation and downstream NF-κB signaling.41, 53, 55 Interestingly, the presence of A20 was shown to result in the accumulation of M1 polyubiquitin at the TNFR1 complex, most likely because A20-ZF7 binding to M1 polyubiquitin chains protects them from cleavage by other DUBs like CYLD.41 A20 also inhibits the activity of several E3 ligases including TRAF6, TRAF2 and cIAP1/2 by preventing their interaction with specific E2 enzymes.61
Although A20 was initially described as a protein that inhibits TNF-induced apoptosis,62 its antiapoptotic effect seems to be much more restricted and dependent on the cellular context than its NF-κB inhibitory function.63 In B cells and dendritic cells (DCs), A20 was even shown to have a proapoptotic function, probably because of its NF-κB inhibitory activity, leading to decreased expression of antiapoptotic proteins.64, 65 Similarly, A20 sensitizes smooth muscle cells to cytokine and Fas-mediated cell death.66 The mechanism by which A20 regulates cell death remains largely unclear. It has been proposed that A20 inhibits TNF-induced cell death by blocking the recruitment of RIPK1 and TRADD to TNFR1, thereby inhibiting subsequent recruitment of FADD and caspase-8.67 Another report suggests that A20 acts by counteracting CUL3-dependent ubiquitination and activation of caspase-8.68 A20 was further shown to ubiquitinate ASK1 upon TNF stimulation, marking it for proteasomal degradation and hereby blocking JNK-mediated apoptosis.69 An important role for A20-ZF7 was established, as reconstitution of A20-deficient MEF cells with a ZF7 mutant protein could not rescue these cells from TNF-induced cell death, most likely because A20 can no longer bind to M1-polyubiquitinated proteins and prevent RIPK1 from forming the cell death-inducing complex II.41, 70 Finally, A20 also restricts ubiquitination of RIPK3 and its binding to RIPK1, protecting cells from necroptosis (Figure 3).71
Regulation of A20 activity
A20 was originally identified as a TNF-responsive gene in human endothelial cells.72 Although A20 is constitutively expressed in some cell types, in most cell types A20 expression is low or absent in resting conditions.63 However, its transcription is rapidly upregulated in an NF-κB-dependent manner in response to various stimuli, thus providing negative feedback control of NF-κB signaling.73 Several other mechanisms contribute to transcriptional regulation of A20. Promoter methylation can result in inactivation of A20, which is mainly observed in different types of lymphomas.74 Depending on the cellular context, expression of A20 can also be up- or downregulated by specific miRNAs. For example, miR125a and miR125b suppress A20 expression in diffuse large B-cell lymphoma, thereby contributing to constitutive NF-κB signaling and tumor cell proliferation.75 In contrast, in sarcoma cells miR29 protects A20 transcripts from degradation by preventing binding of RNA-binding protein HuR and recruitment of the RNA degradation complex.76
At the protein level, A20 is regulated by several post-translational modifications including glycosylation, phosphorylation, ubiquitination and proteolytic cleavage. Under high glucose conditions A20 is O-glycosylated in smooth muscle cells, leading to its subsequent ubiquitination and degradation.77 TNF or LPS stimulation leads to IKKβ-mediated phosphorylation of A20 at Ser381, increasing A20 NF-κB inhibitory potential.78 This is in agreement with the finding that Ser381 phosphorylation increases A20's in vitro DUB activity towards K63 polyubiquitin.50 In lymphocytes, where A20 is constitutively expressed, antigen receptor stimulation induces A20 cleavage by MALT1 at Arg439, followed by its proteasomal degradation.79 Moreover, MALT1-independent proteasomal degradation of A20 has been reported in T cells.80 In this context, RNF114-mediated ubiquitination of A20 was shown to stabilize A20,81 indicating a complex regulatory role for A20 ubiquitination. Finally, A20 DUB activity was shown to be regulated by reversible oxidation of the catalytic cysteine residue in vitro.82
Many A20-interacting proteins are ubiquitin-binding proteins, bridging A20 to its substrates or other ubiquitinated proteins. For example, TAX1BP1 can recruit A20 to K63-ubiquitinated substrates like TRAF6,83, 84 whereas ABIN1 can recruit A20 to M1-ubiquitinated proteins such as NEMO.85
A20 in tissue homeostasis and disease
The important role of A20 in the regulation of NF-κB signaling and cell death is reflected in the phenotype of A20-deficient mice, which die prematurely because of severe multiorgan inflammation.86 Several cell-type-specific A20-deficient mice illustrate the key regulatory role of A20 in different cell types to maintain cellular homeostasis (Table 3). The development of autoimmunity and inflammation may not only reflect enhanced NF-κB or cell death signaling. For example, development of arthritis in myeloid-specific A20-knockout mice reflects the absence of an inhibitory effect of A20 on NLRP3 inflammasome activity and IL-1β ubiquitination, resulting in increased caspase-1-mediated processing of IL-1β.87, 88
Genome-wide association studies identified human A20 as a susceptibility gene for several inflammatory diseases, such as psoriasis, Crohn’s disease, systemic lupus erythematosus (SLE) and rheumatoid arthritis.89 Most single-nucleotide polymorphisms (SNPs) are located up- or downstream of the A20 coding regions or in intronic sequences, indicating increased disease susceptibility by regulating A20 expression. TALEN-mediated genome editing to disrupt specifically the TT>A enhancer region associated with SLE impaired its interaction with the A20 promoter by long-range DNA looping, thereby reducing A20 expression, indicating a causal contribution.90 Two SNPs leading to nonsynonymous mutations in the A20 DUB domain were shown to reduce the NF-κB inhibitory potential of A20 upon overexpression.91 More recently, loss-of-function mutations leading to A20 haploinsufficiency were shown to cause early-onset autoinflammatory disease that resembles Behçet's disease.92 Furthermore, an A20 frameshift mutation that results in a 415 amino-acid protein fragment has been identified in a patient with an autoimmune lymphoproliferative syndrome-like phenotype, and T cells from this patient exhibit increased NF-κB activation.93 Finally, A20 was shown to be a tumor suppressor that is downregulated in several cancers including lymphomas and pancreatic cancer.94
OTULIN
Activity and specificity of OTULIN
OTULIN (OTU DUB with linear linkage specificity), also named FAM105B/Gumby, was discovered in 2013 by two independent groups as the first DUB, which exclusively hydrolyzes M1 polyubiquitin.95, 96 Rivkin et al.96 found that mutations in this protein are causative for an angiogenic phenotype in gumby mice and named it Gumby. Using a bioinformatics approach, Keusekotten et al.95 found OTULIN as a new member of the OTU family that is mostly made up of its OTU domain (Figure 1). The remarkable specificity for M1 polyubiquitin can be explained by two features. First, its high-affinity ubiquitin-binding sites are capable to bind M1 polyubiquitin 100-fold more tightly than structurally similar K63 polyubiquitin. Second, the proximal ubiquitin, more specifically its Glu16 residue, is directly involved in the organization of the catalytic center, where it orients the residues of the catalytic triad in a catalytically active state.95 OTULIN is the first DUB known to apply this mechanism of substrate-assisted catalysis. Such a mechanism suggests that OTULIN targets M1 polyubiquitination in general and not that of specific substrates.
OTULIN in NF-κB signaling and cell death
Different groups have reported that OTULIN antagonizes the generation of M1 polyubiquitin by LUBAC and LUBAC-mediated NF-κB activation.95, 96, 97 The absence of OTULIN results in the accumulation of several M1-ubiquitinated proteins, including LUBAC components, but TNF-induced HOIP recruitment to TNFR1 is not affected. Conversely, ectopic expression of OTULIN leads to delayed TNF-induced NF-κB activation and proinflammatory signaling.95, 97 In the context of TNFR1 signaling, removal of M1 polyubiquitin by OTULIN inhibits the association of NEMO with polyubiquitinated RIPK1.95 Also, expression of a catalytically inactive OTULIN C129A mutant leads to decreased NF-κB activation,95 which can be explained by the ability of this mutant to still bind ubiquitin and to exert a dominant-negative effect. Indeed, Fiil et al.97 provide evidence that a double mutant C129A-W96A, which is catalytically inactive and cannot bind ubiquitin, no longer suppresses NF-κB.95, 97 M1 ubiquitination also protects from TNF-induced cell death by stabilization of complex I.98 Accordingly, stable OTULIN overexpression sensitizes cells to TNF-induced cell death.95 Surprisingly, knockdown of OTULIN, and hence M1 ubiquitin accumulation, also induced cell death.
Next to its effects on TNFR1 signaling, OTULIN regulates NOD2 receptor signaling. NOD2 stimulation induces RIPK2 polyubiquitination by multiple E3 ligases, leading to recruitment of LUBAC, which in turn assembles M1 polyubiquitin on RIPK2 (Figure 2).99 RIPK2 M1 ubiquitination is increased upon knockdown of OTULIN, correlating with enhanced recruitment of NEMO to RIPK2 and an increased NF-κB response.97 Vice versa, overexpression of OTULIN inhibits RIPK2 M1 polyubiquitination and NEMO recruitment.
The role of OTULIN at receptor signaling complexes (e.g. TNFR1 and NOD2 complex) is still rather unclear. Draber et al.41 showed that OTULIN is not recruited to the TNFR1 signaling complex and does not regulate the amount of M1 ubiquitination at the signaling complex itself (e.g. of RIPK1 or NEMO), but rather the amount of cytosolic M1-ubiquitinated proteins including LUBAC components themselves. However, Wagner et al.40 found low levels of endogenous OTULIN in the TNFR1 complex upon TNF stimulation, and the Gyrd-Hansen lab showed that OTULIN regulates RIPK2 ubiquitination at the NOD2 receptor complex.42, 97 Altogether, these data indicate that OTULIN recruitment to receptor signaling complexes might be weak or dynamic.
Regulation of OTULIN activity
OTULIN co-immunoprecipitates with different LUBAC components including HOIP.95, 96 More specifically, OTULIN binds to the PUB domain in HOIP via a conserved PIM domain (Figure 1).100, 101 The interaction is dependent on OTULIN Tyr56 within the PIM motif and HOIP Asn102. Binding of OTULIN to HOIP prevents autoubiquitination of HOIP under basal conditions and is necessary for OTULIN’s ability to antagonize LUBAC-induced NF-κB activity.100 Using a non-binding mutant of HOIP, it was shown that the interaction of HOIP with OTULIN as well as CYLD (see above) is important for TNF-induced NF-κB activation.36 OTULIN and CYLD associate with HOIP in a mutual exclusive manner, indicating that there are two different pools of HOIP, one associated with OTULIN and one with CYLD.41 Tyr56 phosphorylation in the OTULIN PIM domain prevents OTULIN binding to HOIP and hence governs OTULIN function.100 However, kinases and phosphatases involved in this regulation are yet to be determined.
OTULIN in tissue homeostasis and disease
Mice carrying OTULIN loss-of-function mutations are embryonically lethal (E12.5–E14) because of deficient Wnt signaling and vascular defects.96 Recently, the Komander lab generated different conditional OTULIN knockout mice, demonstrating that OTULIN is an essential negative regulator of inflammation and autoimmunity by mediating cell-type-specific effects on M1 ubiquitin signaling (Table 3).102
Patients carrying OTULIN mutations develop a fatal inflammatory syndrome with episodes of systemic inflammation without any evidence of infection.102, 103 This condition, termed otulipenia or OTULIN-related inflammatory syndrome, was treatable with Infliximab (anti-TNF), consistent with the important regulatory function of OTULIN in TNF signaling. Zhou et al.103 identified two missense (Leu272Pro and Tyr244Cys) and one frameshift mutation (Gly174Aspfs*2) in four patients.103 Fibroblasts and PBMCs from these patients show increased NF-κB signaling and inflammatory cytokine production. Damgaard et al.102 showed that Leu272Pro missense mutations in OTULIN found in patients result in reduced stability and activity of OTULIN, consistent with increased M1 polyubiquitin compared with controls.102
Molecular mechanisms determining the non-redundant functions of CYLD, A20 and OTULIN
CYLD, A20 and OTULIN all regulate NF-κB and cell death signaling where they deubiquitinate a number of overlapping substrates (Table 1). One would therefore predict that their function is largely redundant. However, the corresponding knockout mice show significant differences: while A20 or OTULIN-deficient mice are embryonically lethal because of multiorgan inflammation or vascular defects, respectively,86, 96 CYLD-deficient mice show no overall defects in growth and survival.104 Different phenotypes have been observed in the case of cell-type-specific knockout mice. For example, while A20 deficiency in B cells causes B-cell hyperreactivity,65, 105 reported consequences of CYLD deficiency are controversial, ranging from an absence of effects to marked B-cell hyperplasia.65, 105, 106, 107, 108 These differences could reflect varying compensation for the loss of CYLD function by A20. However, compound loss of A20 and CYLD did not exacerbate the effects of A20 deficiency,105 indicating that the discrepancy of the various reported effects of CYLD deficiency is not due to functional compensation by A20.
The non-redundant function of CYLD, A20 and OTULIN can be partially explained by their different specificity for various types of polyubiquitin. In vitro DUB assays revealed that both, CYLD and OTULIN hydrolyze M1 polyubiquitin, while CYLD additionally cleaves K63 polyubiquitin and with lower preference K11 and K48 polyubiquitin. A20 can cleave K48 and K11 polyubiquitin and less efficiently K63 polyubiquitin in vitro.8, 47 However, ubiquitin chain specificity of DUBs may be different in a specific cellular context, which is demonstrated by the fact that A20 phosphorylation by IKKβ increases its DUB activity towards K63 polyubiquitin.50 Recent evidence suggests that the recognition of different linkages by DUBs is differentially regulated by the presence of specific types of polyubiquitin branching. More specifically, K48–K63 branching protects K63 linkages from CYLD-mediated deubiquitination, while the activity of A20 is not affected.3 A20-mediated K63 deubiquitination is, however, inhibited by M1 polyubiquitination, either mixed or branched with K63.50 Finally, it is possible that the ubiquitin chain specificity of different DUBs differs depending on the substrate and cellular context, including the presence and binding of adaptor proteins (e.g. TAX1BP1, ABINs, OPTN, p62) that recruit DUBs to specific ubiquitinated substrates.33, 34, 83, 84, 85
In addition to different polyubiquitin chain specificities, deubiquitination-independent activities may contribute to the non-redundant function of CYLD, A20 and OTULIN. In the case of A20, this may involve its E3 ligase activity,49 either directly or indirectly by interacting with other E3 ligases. Moreover, binding of DUBs to specific proteins or different types of polyubiquitin can affect the formation or stability of signaling complexes. Such non-catalytic mechanisms of action have already been shown for A20,41, 55, 61 and could create a functional niche also for CYLD and OTULIN.
Spatial and temporal differences in expression of CYLD, A20 and OTULIN may also explain their non-redundant functions. In contrast to CYLD and OTULIN, A20 is not or only weakly expressed in most resting cells, and needs to be transcriptionally upregulated upon cellular stimulation in an NF-κB-dependent manner. Therefore, it can be postulated that CYLD and OTULIN regulate basal ubiquitination in unstimulated cells to prevent aberrant signal transduction and dampen early responses, whereas A20 is more critical to the negative feedback regulation and termination of immune signaling. For instance, OTULIN associates with LUBAC in unstimulated cells, and absence of OTULIN leads to accumulation of M1-ubiquitinated proteins and constitutive NF-κB activation.102 However, there is substantial evidence that CYLD and OTULIN not only impact signaling under baseline conditions but also at the level of receptor signaling complexes that are formed upon stimulation.40, 42, 97 Finally and as already described in previous sections, inducible and cell-type-specific expression of miRNAs, as well as post-translational modifications, may contribute to spatial and temporal differences in expression and activity of specific DUBs.
Conclusion and Future Perspectives
It is clear that NF-κB activation and cell death are controlled by a tight regulatory network of DUBs to ensure optimal signal transduction and immune homeostasis. The elucidation of novel and complex types of ubiquitination can be expected to further reveal specific functions and mechanisms of action of CYLD, A20 and OTULIN, as well as their crosstalk with each other or other DUBs. In addition, the careful analysis of conditional DUB-specific knockout and knock-in mice, as well as patients carrying specific mutations, is likely to reveal novel DUB functions that may reach far beyond inflammation and immunity, which is already described in the case of CYLD. As A20, CYLD and OTULIN have all been implicated in inflammatory diseases or cancer, the ultimate challenge will be to translate this fundamental knowledge in novel and better therapies.
References
Komander D, Rape M . The ubiquitin code. Annu Rev Biochem 2012; 81: 203–229.
Emmerich CH, Ordureau A, Strickson S, Arthur JS, Pedrioli PG, Komander D et al. Activation of the canonical IKK complex by K63/M1-linked hybrid ubiquitin chains. Proc Natl Acad Sci USA 2013; 110: 15247–15252.
Ohtake F, Saeki Y, Ishido S, Kanno J, Tanaka K . The K48-K63 branched ubiquitin chain regulates NF-kappaB signaling. Mol Cell 2016; 64: 251–266.
Abdul Rehman SA, Kristariyanto YA, Choi SY, Nkosi PJ, Weidlich S, Labib K et al. MINDY-1 is a member of an evolutionarily conserved and structurally distinct new family of deubiquitinating enzymes. Mol Cell 2016; 63: 146–155.
Heideker J, Wertz IE . DUBs, the regulation of cell identity and disease. Biochem J 2015; 467: 191.
Harhaj EW, Dixit VM . Regulation of NF-kappaB by deubiquitinases. Immunol Rev 2012; 246: 107–124.
Saito K, Kigawa T, Koshiba S, Sato K, Matsuo Y, Sakamoto A et al. The CAP-Gly domain of CYLD associates with the proline-rich sequence in NEMO/IKKgamma. Structure 2004; 12: 1719–1728.
Ritorto MS, Ewan R, Perez-Oliva AB, Knebel A, Buhrlage SJ, Wightman M et al. Screening of DUB activity and specificity by MALDI-TOF mass spectrometry. Nat Commun 2014; 5: 4763.
Komander D, Lord CJ, Scheel H, Swift S, Hofmann K, Ashworth A et al. The structure of the CYLD USP domain explains its specificity for Lys63-linked polyubiquitin and reveals a B box module. Mol Cell 2008; 29: 451–464.
Komander D, Reyes-Turcu F, Licchesi JD, Odenwaelder P, Wilkinson KD, Barford D . Molecular discrimination of structurally equivalent Lys 63-linked and linear polyubiquitin chains. EMBO Rep 2009; 10: 466–473.
Sato Y, Goto E, Shibata Y, Kubota Y, Yamagata A, Goto-Ito S et al. Structures of CYLD USP with Met1- or Lys63-linked diubiquitin reveal mechanisms for dual specificity. Nat Struct Mol Biol 2015; 22: 222–229.
Brummelkamp TR, Nijman SM, Dirac AM, Bernards R . Loss of the cylindromatosis tumour suppressor inhibits apoptosis by activating NF-kappaB. Nature 2003; 424: 797–801.
Kovalenko A, Chable-Bessia C, Cantarella G, Israel A, Wallach D, Courtois G . The tumour suppressor CYLD negatively regulates NF-kappaB signalling by deubiquitination. Nature 2003; 424: 801–805.
Trompouki E, Hatzivassiliou E, Tsichritzis T, Farmer H, Ashworth A, Mosialos G . CYLD is a deubiquitinating enzyme that negatively regulates NF-kappaB activation by TNFR family members. Nature 2003; 424: 793–796.
Hitomi J, Christofferson DE, Ng A, Yao J, Degterev A, Xavier RJ et al. Identification of a molecular signaling network that regulates a cellular necrotic cell death pathway. Cell 2008; 135: 1311–1323.
O'Donnell MA, Perez-Jimenez E, Oberst A, Ng A, Massoumi R, Xavier R et al. Caspase 8 inhibits programmed necrosis by processing CYLD. Nat Cell Biol 2011; 13: 1437–1442.
Moquin DM, McQuade T, Chan FK . CYLD deubiquitinates RIP1 in the TNFalpha-induced necrosome to facilitate kinase activation and programmed necrosis. PLoS ONE 2013; 8: e76841.
Schworer SA, Smirnova II, Kurbatova I, Bagina U, Churova M, Fowler T et al. Toll-like receptor-mediated down-regulation of the deubiquitinase cylindromatosis (CYLD) protects macrophages from necroptosis in wild-derived mice. J Biol Chem 2014; 289: 14422–14433.
Legarda D, Justus SJ, Ang RL, Rikhi N, Li W, Moran TM et al. CYLD proteolysis protects macrophages from TNF-mediated auto-necroptosis induced by LPS and licensed by type I IFN. Cell Rep 2016; 15: 2449–2461.
Mathis BJ, Lai Y, Qu C, Janicki JS, Cui T . CYLD-mediated signaling and diseases. Curr Drug Targets 2015; 16: 284–294.
Sun SC . CYLD: a tumor suppressor deubiquitinase regulating NF-kappaB activation and diverse biological processes. Cell Death Differ 2010; 17: 25–34.
Jono H, Lim JH, Chen LF, Xu H, Trompouki E, Pan ZK et al. NF-kappaB is essential for induction of CYLD, the negative regulator of NF-kappaB: evidence for a novel inducible autoregulatory feedback pathway. J Biol Chem 2004; 279: 36171–36174.
Ye H, Liu X, Lv M, Wu Y, Kuang S, Gong J et al. MicroRNA and transcription factor co-regulatory network analysis reveals miR-19 inhibits CYLD in T-cell acute lymphoblastic leukemia. Nucleic Acids Res 2012; 40: 5201–5214.
Reiley W, Zhang M, Wu X, Granger E, Sun SC . Regulation of the deubiquitinating enzyme CYLD by IkappaB kinase gamma-dependent phosphorylation. Mol Cell Biol 2005; 25: 3886–3895.
Hutti JE, Shen RR, Abbott DW, Zhou AY, Sprott KM, Asara JM et al. Phosphorylation of the tumor suppressor CYLD by the breast cancer oncogene IKKepsilon promotes cell transformation. Mol Cell 2009; 34: 461–472.
Gringhuis SI, Kaptein TM, Wevers BA, Mesman AW, Geijtenbeek TB . Fucose-specific DC-SIGN signalling directs T helper cell type-2 responses via IKKepsilon- and CYLD-dependent Bcl3 activation. Nat Commun 2014; 5: 3898.
Thein S, Pham A, Bayer KU, Tao-Cheng JH, Dosemeci A . IKK regulates the deubiquitinase CYLD at the postsynaptic density. Biochem Biophys Res Commun 2014; 450: 550–554.
Staal J, Driege Y, Bekaert T, Demeyer A, Muyllaert D, Van Damme P et al. T-cell receptor-induced JNK activation requires proteolytic inactivation of CYLD by MALT1. EMBO J 2011; 30: 1742–1752.
Arora M, Kaul D, Varma N, Marwaha RK . Cellular proteolytic modification of tumor-suppressor CYLD is critical for the initiation of human T-cell acute lymphoblastic leukemia. Blood Cells Mol Dis 2015; 54: 132–138.
Klei LR, Hu D, Panek R, Alfano DN, Bridwell RE, Bailey KM et al. MALT1 protease activation triggers acute disruption of endothelial barrier integrity via CYLD cleavage. Cell Rep 2016; 17: 221–232.
Wu X, Fukushima H, North BJ, Nagaoka Y, Nagashima K, Deng F et al. SCFbeta-TRCP regulates osteoclastogenesis via promoting CYLD ubiquitination. Oncotarget 2014; 5: 4211–4221.
Kobayashi T, Masoumi KC, Massoumi R . Deubiquitinating activity of CYLD is impaired by SUMOylation in neuroblastoma cells. Oncogene 2015; 34: 2251–2260.
Jin W, Chang M, Paul EM, Babu G, Lee AJ, Reiley W et al. Deubiquitinating enzyme CYLD negatively regulates RANK signaling and osteoclastogenesis in mice. J Clin Invest 2008; 118: 1858–1866.
Nagabhushana A, Bansal M, Swarup G . Optineurin is required for CYLD-dependent inhibition of TNFalpha-induced NF-kappaB activation. PLoS ONE 2011; 6: e17477.
Ahmed N, Zeng M, Sinha I, Polin L, Wei WZ, Rathinam C et al. The E3 ligase Itch and deubiquitinase Cyld act together to regulate Tak1 and inflammation. Nat Immunol 2011; 12: 1176–1183.
Takiuchi T, Nakagawa T, Tamiya H, Fujita H, Sasaki Y, Saeki Y et al. Suppression of LUBAC-mediated linear ubiquitination by a specific interaction between LUBAC and the deubiquitinases CYLD and OTULIN. Genes Cells 2014; 19: 254–272.
Elliott PR, Leske D, Hrdinka M, Bagola K, Fiil BK, McLaughlin SH et al. SPATA2 links CYLD to LUBAC, activates CYLD, and controls LUBAC signaling. Mol Cell 2016; 63: 990–1005.
Kupka S, De Miguel D, Draber P, Martino L, Surinova S, Rittinger K et al. SPATA2-mediated binding of CYLD to HOIP enables CYLD recruitment to signaling complexes. Cell Rep 2016; 16: 2271–2280.
Schlicher L, Wissler M, Preiss F, Brauns-Schubert P, Jakob C, Dumit V et al. SPATA2 promotes CYLD activity and regulates TNF-induced NF-kappaB signaling and cell death. EMBO Rep 2016; 17: 1485–1497.
Wagner SA, Satpathy S, Beli P, Choudhary C . SPATA2 links CYLD to the TNF-alpha receptor signaling complex and modulates the receptor signaling outcomes. EMBO J 2016; 35: 1868–1884.
Draber P, Kupka S, Reichert M, Draberova H, Lafont E, de Miguel D et al. LUBAC-recruited CYLD and A20 regulate gene activation and cell death by exerting opposing effects on linear ubiquitin in signaling complexes. Cell Rep 2015; 13: 2258–2272.
Hrdinka M, Fiil BK, Zucca M, Leske D, Bagola K, Yabal M et al. CYLD limits Lys63- and Met1-linked ubiquitin at receptor complexes to regulate innate immune signaling. Cell Rep 2016; 14: 2846–2858.
Bignell GR, Warren W, Seal S, Takahashi M, Rapley E, Barfoot R et al. Identification of the familial cylindromatosis tumour-suppressor gene. Nat Genet 2000; 25: 160–165.
Massoumi R . CYLD: a deubiquitination enzyme with multiple roles in cancer. Fut Oncol 2011; 7: 285–297.
Cleynen I, Vazeille E, Artieda M, Verspaget HW, Szczypiorska M, Bringer MA et al. Genetic and microbial factors modulating the ubiquitin proteasome system in inflammatory bowel disease. Gut 2014; 63: 1265–1274.
Evans PC, Ovaa H, Hamon M, Kilshaw PJ, Hamm S, Bauer S et al. Zinc-finger protein A20, a regulator of inflammation and cell survival, has de-ubiquitinating activity. Biochem J 2004; 378: 727–734.
Komander D, Barford D . Structure of the A20 OTU domain and mechanistic insights into deubiquitination. Biochem J 2008; 409: 77–85.
Boone DL, Turer EE, Lee EG, Ahmad RC, Wheeler MT, Tsui C et al. The ubiquitin-modifying enzyme A20 is required for termination of Toll-like receptor responses. Nat Immunol 2004; 5: 1052–1060.
Wertz IE, O'Rourke KM, Zhou H, Eby M, Aravind L, Seshagiri S et al. De-ubiquitination and ubiquitin ligase domains of A20 downregulate NF-kappaB signalling. Nature 2004; 430: 694–699.
Wertz IE, Newton K, Seshasayee D, Kusam S, Lam C, Zhang J et al. Phosphorylation and linear ubiquitin direct A20 inhibition of inflammation. Nature 2015; 528: 370–375.
Shembade N, Harhaj NS, Parvatiyar K, Copeland NG, Jenkins NA, Matesic LE et al. The E3 ligase Itch negatively regulates inflammatory signaling pathways by controlling the function of the ubiquitin-editing enzyme A20. Nat Immunol 2008; 9: 254–262.
Shembade N, Parvatiyar K, Harhaj NS, Harhaj EW . The ubiquitin-editing enzyme A20 requires RNF11 to downregulate NF-kappaB signalling. EMBO J 2009; 28: 513–522.
Bosanac I, Wertz IE, Pan B, Yu C, Kusam S, Lam C et al. Ubiquitin binding to A20 ZnF4 is required for modulation of NF-kappaB signaling. Mol Cell 2010; 40: 548–557.
Tokunaga F, Nishimasu H, Ishitani R, Goto E, Noguchi T, Mio K et al. Specific recognition of linear polyubiquitin by A20 zinc finger 7 is involved in NF-kappaB regulation. EMBO J 2012; 31: 3856–3870.
Verhelst K, Carpentier I, Kreike M, Meloni L, Verstrepen L, Kensche T et al. A20 inhibits LUBAC-mediated NF-kappaB activation by binding linear polyubiquitin chains via its zinc finger 7. EMBO J 2012; 31: 3845–3855.
Catrysse L, Vereecke L, Beyaert R, van Loo G . A20 in inflammation and autoimmunity. Trends Immunol 2014; 35: 22–31.
De A, Dainichi T, Rathinam CV, Ghosh S . The deubiquitinase activity of A20 is dispensable for NF-kappaB signaling. EMBO Rep 2014; 15: 775–783.
Lu TT, Onizawa M, Hammer GE, Turer EE, Yin Q, Damko E et al. Dimerization and ubiquitin mediated recruitment of A20, a complex deubiquitinating enzyme. Immunity 2013; 38: 896–905.
Verhelst K, van Loo G, Beyaert R . A20: attractive without showing cleavage. EMBO Rep 2014; 15: 734–735.
Skaug B, Chen J, Du F, He J, Ma A, Chen ZJ . Direct, noncatalytic mechanism of IKK inhibition by A20. Mol Cell 2011; 44: 559–571.
Shembade N, Ma A, Harhaj EW . Inhibition of NF-kappaB signaling by A20 through disruption of ubiquitin enzyme complexes. Science 2010; 327: 1135–1139.
Opipari AW Jr., Hu HM, Yabkowitz R, Dixit VM . The A20 zinc finger protein protects cells from tumor necrosis factor cytotoxicity. J Biol Chem 1992; 267: 12424–12427.
Verstrepen L, Verhelst K, van Loo G, Carpentier I, Ley SC, Beyaert R . Expression, biological activities and mechanisms of action of A20 (TNFAIP3). Biochem Pharmacol 2010; 80: 2009–2020.
Kool M, van Loo G, Waelput W, De Prijck S, Muskens F, Sze M et al. The ubiquitin-editing protein A20 prevents dendritic cell activation, recognition of apoptotic cells, and systemic autoimmunity. Immunity 2011; 35: 82–96.
Tavares RM, Turer EE, Liu CL, Advincula R, Scapini P, Rhee L et al. The ubiquitin modifying enzyme A20 restricts B cell survival and prevents autoimmunity. Immunity 2010; 33: 181–191.
Daniel S, Patel VI, Shrikhande GV, Scali ST, Ramsey HE, Csizmadia E et al. The universal NF-kappaB inhibitor a20 protects from transplant vasculopathy by differentially affecting apoptosis in endothelial and smooth muscle cells. Transplant Proc 2006; 38: 3225–3227.
He KL, Ting AT . A20 inhibits tumor necrosis factor (TNF) alpha-induced apoptosis by disrupting recruitment of TRADD and RIP to the TNF receptor 1 complex in Jurkat T cells. Mol Cell Biol 2002; 22: 6034–6045.
Jin Z, Li Y, Pitti R, Lawrence D, Pham VC, Lill JR et al. Cullin3-based polyubiquitination and p62-dependent aggregation of caspase-8 mediate extrinsic apoptosis signaling. Cell 2009; 137: 721–735.
Won M, Park KA, Byun HS, Sohn KC, Kim YR, Jeon J et al. Novel anti-apoptotic mechanism of A20 through targeting ASK1 to suppress TNF-induced JNK activation. Cell Death Differ 2010; 17: 1830–1841.
Yamaguchi N, Yamaguchi N . The seventh zinc finger motif of A20 is required for the suppression of TNF-alpha-induced apoptosis. FEBS Lett 2015; 589: 1369–1375.
Onizawa M, Oshima S, Schulze-Topphoff U, Oses-Prieto JA, Lu T, Tavares R et al. The ubiquitin-modifying enzyme A20 restricts ubiquitination of the kinase RIPK3 and protects cells from necroptosis. Nat Immunol 2015; 16: 618–627.
Dixit VM, Green S, Sarma V, Holzman LB, Wolf FW, O'Rourke K et al. Tumor necrosis factor-alpha induction of novel gene products in human endothelial cells including a macrophage-specific chemotaxin. J Biol Chem 1990; 265: 2973–2978.
Krikos A, Laherty CD, Dixit VM . Transcriptional activation of the tumor necrosis factor alpha-inducible zinc finger protein, A20, is mediated by kappa B elements. J Biol Chem 1992; 267: 17971–17976.
Chanudet E, Huang Y, Ichimura K, Dong G, Hamoudi RA, Radford J et al. A20 is targeted by promoter methylation, deletion and inactivating mutation in MALT lymphoma. Leukemia 2010; 24: 483–487.
Kim SW, Ramasamy K, Bouamar H, Lin AP, Jiang D, Aguiar RC . MicroRNAs miR-125a and miR-125b constitutively activate the NF-kappaB pathway by targeting the tumor necrosis factor alpha-induced protein 3 (TNFAIP3, A20). Proc Natl Acad Sci USA 2012; 109: 7865–7870.
Balkhi MY, Iwenofu OH, Bakkar N, Ladner KJ, Chandler DS, Houghton PJ et al. miR-29 acts as a decoy in sarcomas to protect the tumor suppressor A20 mRNA from degradation by HuR. Sci Signal 2013; 6: ra63.
Shrikhande GV, Scali ST, da Silva CG, Damrauer SM, Csizmadia E, Putheti P et al. O-glycosylation regulates ubiquitination and degradation of the anti-inflammatory protein A20 to accelerate atherosclerosis in diabetic ApoE-null mice. PLoS ONE 2010; 5: e14240.
Hutti JE, Turk BE, Asara JM, Ma A, Cantley LC, Abbott DW . IkappaB kinase beta phosphorylates the K63 deubiquitinase A20 to cause feedback inhibition of the NF-kappaB pathway. Mol Cell Biol 2007; 27: 7451–7461.
Coornaert B, Baens M, Heyninck K, Bekaert T, Haegman M, Staal J et al. T cell antigen receptor stimulation induces MALT1 paracaspase-mediated cleavage of the NF-kappaB inhibitor A20. Nat Immunol 2008; 9: 263–271.
Duwel M, Welteke V, Oeckinghaus A, Baens M, Kloo B, Ferch U et al. A20 negatively regulates T cell receptor signaling to NF-kappaB by cleaving Malt1 ubiquitin chains. J Immunol 2009; 182: 7718–7728.
Rodriguez MS, Egana I, Lopitz-Otsoa F, Aillet F, Lopez-Mato MP, Dorronsoro A et al. The RING ubiquitin E3 RNF114 interacts with A20 and modulates NF-kappaB activity and T-cell activation. Cell Death Dis 2014; 5: e1399.
Kulathu Y, Garcia FJ, Mevissen TE, Busch M, Arnaudo N, Carroll KS et al. Regulation of A20 and other OTU deubiquitinases by reversible oxidation. Nat Commun 2013; 4: 1569.
Iha H, Peloponese JM, Verstrepen L, Zapart G, Ikeda F, Smith CD et al. Inflammatory cardiac valvulitis in TAX1BP1-deficient mice through selective NF-kappaB activation. EMBO J 2008; 27: 629–641.
Shembade N, Harhaj NS, Liebl DJ, Harhaj EW . Essential role for TAX1BP1 in the termination of TNF-alpha-, IL-1- and LPS-mediated NF-kappaB and JNK signaling. EMBO J 2007; 26: 3910–3922.
Wagner S, Carpentier I, Rogov V, Kreike M, Ikeda F, Lohr F et al. Ubiquitin binding mediates the NF-kappaB inhibitory potential of ABIN proteins. Oncogene 2008; 27: 3739–3745.
Lee EG, Boone DL, Chai S, Libby SL, Chien M, Lodolce JP et al. Failure to regulate TNF-induced NF-kappaB and cell death responses in A20-deficient mice. Science 2000; 289: 2350–2354.
Duong BH, Onizawa M, Oses-Prieto JA, Advincula R, Burlingame A, Malynn BA et al. A20 restricts ubiquitination of pro-interleukin-1beta protein complexes and suppresses NLRP3 inflammasome activity. Immunity 2015; 42: 55–67.
Vande Walle L, Van Opdenbosch N, Jacques P, Fossoul A, Verheugen E, Vogel P et al. Negative regulation of the NLRP3 inflammasome by A20 protects against arthritis. Nature 2014; 512: 69–73.
Vereecke L, Beyaert R, van Loo G . Genetic relationships between A20/TNFAIP3, chronic inflammation and autoimmune disease. Biochem Soc Trans 2011; 39: 1086–1091.
Wang S, Wen F, Tessneer KL, Gaffney PM . TALEN-mediated enhancer knockout influences TNFAIP3 gene expression and mimics a molecular phenotype associated with systemic lupus erythematosus. Genes Immun 2016; 17: 165–170.
Lodolce JP, Kolodziej LE, Rhee L, Kariuki SN, Franek BS, McGreal NM et al. African-derived genetic polymorphisms in TNFAIP3 mediate risk for autoimmunity. J Immunol 2010; 184: 7001–7009.
Zhou Q, Wang H, Schwartz DM, Stoffels M, Park YH, Zhang Y et al. Loss-of-function mutations in TNFAIP3 leading to A20 haploinsufficiency cause an early-onset autoinflammatory disease. Nat Genet 2016; 48: 67–73.
Takagi M, Ogata S, Ueno H, Yoshida K, Yeh T, Hoshino A et al. Haploinsufficiency of TNFAIP3 (A20) by germline mutation is involved in autoimmune lymphoproliferative syndrome. J Allergy Clin Immunol 2016; S0091-6749: 31286–31286.
Zhang F, Yang L, Li Y . The role of A20 in the pathogenesis of lymphocytic malignancy. Cancer Cell Int 2012; 12: 44.
Keusekotten K, Elliott PR, Glockner L, Fiil BK, Damgaard RB, Kulathu Y et al. OTULIN antagonizes LUBAC signaling by specifically hydrolyzing Met1-linked polyubiquitin. Cell 2013; 153: 1312–1326.
Rivkin E, Almeida SM, Ceccarelli DF, Juang YC, MacLean TA, Srikumar T et al. The linear ubiquitin-specific deubiquitinase gumby regulates angiogenesis. Nature 2013; 498: 318–324.
Fiil BK, Damgaard RB, Wagner SA, Keusekotten K, Fritsch M, Bekker-Jensen S et al. OTULIN restricts Met1-linked ubiquitination to control innate immune signaling. Mol Cell 2013; 50: 818–830.
Haas TL, Emmerich CH, Gerlach B, Schmukle AC, Cordier SM, Rieser E et al. Recruitment of the linear ubiquitin chain assembly complex stabilizes the TNF-R1 signaling complex and is required for TNF-mediated gene induction. Mol Cell 2009; 36: 831–844.
Damgaard RB, Nachbur U, Yabal M, Wong WW, Fiil BK, Kastirr M et al. The ubiquitin ligase XIAP recruits LUBAC for NOD2 signaling in inflammation and innate immunity. Mol Cell 2012; 46: 746–758.
Elliott PR, Nielsen SV, Marco-Casanova P, Fiil BK, Keusekotten K, Mailand N et al. Molecular basis and regulation of OTULIN-LUBAC interaction. Mol Cell 2014; 54: 335–348.
Schaeffer V, Akutsu M, Olma MH, Gomes LC, Kawasaki M, Dikic I . Binding of OTULIN to the PUB domain of HOIP controls NF-kappaB signaling. Mol Cell 2014; 54: 349–361.
Damgaard RB, Walker JA, Marco-Casanova P, Morgan NV, Titheradge HL, Elliott PR et al. The Deubiquitinase OTULIN Is an Essential Negative Regulator of Inflammation and Autoimmunity. Cell 2016; 166: 1215–1230 e1220.
Zhou Q, Yu X, Demirkaya E, Deuitch N, Stone D, Tsai WL et al. Biallelic hypomorphic mutations in a linear deubiquitinase define otulipenia, an early-onset autoinflammatory disease. Proc Natl Acad Sci USA 2016; 113: 10127–10132.
Reiley WW, Zhang M, Jin W, Losiewicz M, Donohue KB, Norbury CC et al. Regulation of T cell development by the deubiquitinating enzyme CYLD. Nat Immunol 2006; 7: 411–417.
Chu Y, Soberon V, Glockner L, Beyaert R, Massoumi R, van Loo G et al. A20 and CYLD do not share significant overlapping functions during B cell development and activation. J Immunol 2012; 189: 4437–4443.
Jin W, Reiley WR, Lee AJ, Wright A, Wu X, Zhang M et al. Deubiquitinating enzyme CYLD regulates the peripheral development and naive phenotype maintenance of B cells. J Biol Chem 2007; 282: 15884–15893.
Massoumi R, Chmielarska K, Hennecke K, Pfeifer A, Fassler R . Cyld inhibits tumor cell proliferation by blocking Bcl-3-dependent NF-kappaB signaling. Cell 2006; 125: 665–677.
Zhang J, Stirling B, Temmerman ST, Ma CA, Fuss IJ, Derry JM et al. Impaired regulation of NF-kappaB and increased susceptibility to colitis-associated tumorigenesis in CYLD-deficient mice. J Clin Invest 2006; 116: 3042–3049.
Reiley WW, Jin W, Lee AJ, Wright A, Wu X, Tewalt EF et al. Deubiquitinating enzyme CYLD negatively regulates the ubiquitin-dependent kinase Tak1 and prevents abnormal T cell responses. J Exp Med 2007; 204: 1475–1485.
Wex K, Schmid U, Just S, Wang X, Wurm R, Naumann M et al. Receptor-interacting protein kinase-2 inhibition by CYLD impairs antibacterial immune responses in macrophages. Front Immunol 2015; 6: 650.
Wright A, Reiley WW, Chang M, Jin W, Lee AJ, Zhang M et al. Regulation of early wave of germ cell apoptosis and spermatogenesis by deubiquitinating enzyme CYLD. Dev Cell 2007; 13: 705–716.
Yoshida H, Jono H, Kai H, Li JD . The tumor suppressor cylindromatosis (CYLD) acts as a negative regulator for toll-like receptor 2 signaling via negative cross-talk with TRAF6 AND TRAF7. J Biol Chem 2005; 280: 41111–41121.
Hitotsumatsu O, Ahmad RC, Tavares R, Wang M, Philpott D, Turer EE et al. The ubiquitin-editing enzyme A20 restricts nucleotide-binding oligomerization domain containing 2-triggered signals. Immunity 2008; 28: 381–390.
Mauro C, Pacifico F, Lavorgna A, Mellone S, Iannetti A, Acquaviva R et al. ABIN-1 binds to NEMO/IKKgamma and co-operates with A20 in inhibiting NF-kappaB. J Biol Chem 2006; 281: 18482–18488.
Stilo R, Varricchio E, Liguoro D, Leonardi A, Vito P . A20 is a negative regulator of BCL10- and CARMA3-mediated activation of NF-kappaB. J Cell Sci 2008; 121: 1165–1171.
Lee AJ, Zhou X, Chang M, Hunzeker J, Bonneau RH, Zhou D et al. Regulation of natural killer T-cell development by deubiquitinase CYLD. EMBO J 2010; 29: 1600–1612.
Friedman CS, O'Donnell MA, Legarda-Addison D, Ng A, Cardenas WB, Yount JS et al. The tumour suppressor CYLD is a negative regulator of RIG-I-mediated antiviral response. EMBO Rep 2008; 9: 930–936.
Trompouki E, Tsagaratou A, Kosmidis SK, Dolle P, Qian J, Kontoyiannis DL et al. Truncation of the catalytic domain of the cylindromatosis tumor suppressor impairs lung maturation. Neoplasia 2009; 11: 469–476.
Nikolaou K, Tsagaratou A, Eftychi C, Kollias G, Mosialos G, Talianidis I . Inactivation of the deubiquitinase CYLD in hepatocytes causes apoptosis, inflammation, fibrosis, and cancer. Cancer Cell 2012; 21: 738–750.
Jin YJ, Wang S, Cho J, Selim MA, Wright T, Mosialos G et al. Epidermal CYLD inactivation sensitizes mice to the development of sebaceous and basaloid skin tumors. JCI Insight 2016; 1: e86548.
Karatzas DN, Xanthopoulos K, Kotantaki P, Pseftogas A, Teliousis K, Hatzivassiliou EG et al. Inactivation of CYLD in intestinal epithelial cells exacerbates colitis-associated colorectal carcinogenesis – a short report. Cell Oncol (Dordr) 2016; 39: 287–293.
Reissig S, Hovelmeyer N, Weigmann B, Nikolaev A, Kalt B, Wunderlich TF et al. The tumor suppressor CYLD controls the function of murine regulatory T cells. J Immunol 2012; 189: 4770–4776.
Hovelmeyer N, Wunderlich FT, Massoumi R, Jakobsen CG, Song J, Worns MA et al. Regulation of B cell homeostasis and activation by the tumor suppressor gene CYLD. J Exp Med 2007; 204: 2615–2627.
Srokowski CC, Masri J, Hovelmeyer N, Krembel AK, Tertilt C, Strand D et al. Naturally occurring short splice variant of CYLD positively regulates dendritic cell function. Blood 2009; 113: 5891–5895.
Reissig S, Hovelmeyer N, Tang Y, Weih D, Nikolaev A, Riemann M et al. The deubiquitinating enzyme CYLD regulates the differentiation and maturation of thymic medullary epithelial cells. Immunol Cell Biol 2015; 93: 558–566.
Vereecke L, Sze M, Mc Guire C, Rogiers B, Chu Y, Schmidt-Supprian M et al. Enterocyte-specific A20 deficiency sensitizes to tumor necrosis factor-induced toxicity and experimental colitis. J Exp Med 2010; 207: 1513–1523.
Matmati M, Jacques P, Maelfait J, Verheugen E, Kool M, Sze M et al. A20 (TNFAIP3) deficiency in myeloid cells triggers erosive polyarthritis resembling rheumatoid arthritis. Nat Genet 2011; 43: 908–912.
Maelfait J, Roose K, Bogaert P, Sze M, Saelens X, Pasparakis M et al. A20 (Tnfaip3) deficiency in myeloid cells protects against influenza A virus infection. PLoS Pathog 2012; 8: e1002570.
Hammer GE, Turer EE, Taylor KE, Fang CJ, Advincula R, Oshima S et al. Expression of A20 by dendritic cells preserves immune homeostasis and prevents colitis and spondyloarthritis. Nat Immunol 2011; 12: 1184–1193.
Maelfait J, Roose K, Vereecke L, Mc Guire C, Sze M, Schuijs MJ et al. A20 Deficiency in Lung Epithelial Cells Protects against Influenza A Virus Infection. PLoS Pathog 2016; 12: e1005410.
Lippens S, Lefebvre S, Gilbert B, Sze M, Devos M, Verhelst K et al. Keratinocyte-specific ablation of the NF-kappaB regulatory protein A20 (TNFAIP3) reveals a role in the control of epidermal homeostasis. Cell Death Differ 2011; 18: 1845–1853.
Mc Guire C, Rahman M, Schwaninger M, Beyaert R, van Loo G . The ubiquitin editing enzyme A20 (TNFAIP3) is upregulated during permanent middle cerebral artery occlusion but does not influence disease outcome. Cell Death Dis 2013; 4: e531.
Wang X, Deckert M, Xuan NT, Nishanth G, Just S, Waisman A et al. Astrocytic A20 ameliorates experimental autoimmune encephalomyelitis by inhibiting NF-kappaB- and STAT1-dependent chemokine production in astrocytes. Acta Neuropathol 2013; 126: 711–772.
Vereecke L, Vieira-Silva S, Billiet T, van Es JH, Mc Guire C, Slowicka K et al. A20 controls intestinal homeostasis through cell-specific activities. Nat Commun 2014; 5: 5103.
Drennan MB, Govindarajan S, Verheugen E, Coquet JM, Staal J, McGuire C et al. NKT sublineage specification and survival requires the ubiquitin-modifying enzyme TNFAIP3/A20. J Exp Med 2016; 213: 1973–1981.
Acknowledgements
This work was supported by grants from the Fund for Scientific Research Flanders (FWO), the Belgian Foundation Against Cancer, Interuniversity Attraction Poles, Concerted Research Actions (GOA) and the Group-ID Multidisciplinary Research Partnership of Ghent University. ML is supported by a predoctoral fellowship from the FWO.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by M Gyrd-Hansen
Rights and permissions
About this article
Cite this article
Lork, M., Verhelst, K. & Beyaert, R. CYLD, A20 and OTULIN deubiquitinases in NF-κB signaling and cell death: so similar, yet so different. Cell Death Differ 24, 1172–1183 (2017). https://doi.org/10.1038/cdd.2017.46
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cdd.2017.46