Abstract
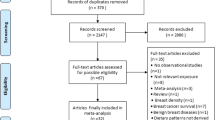
Lifestyle factors related to energy balance, such as excess body weight, poor diet, and physical inactivity, are associated with risk of sporadic endometrial cancer (EC) and colorectal cancer (CRC). There are limited data on energy balance-related lifestyle factors and EC or CRC risk among individuals with lynch syndrome, who are at extraordinarily higher risk of developing EC or CRC. We conducted a systematic review of evidence related to weight status, weight change, dietary habits, and physical activity on EC and CRC risk among individuals with lynch syndrome. Findings are reported narratively. We searched Medline, EMBASE, CENTRAL, PubMed, and clinicaltrials.gov up to June 14th, 2018. In total, 1060 studies were identified and 16 were included. Three studies were related to EC and 13 to CRC. Overall, evidence suggests that weight status/weight change may not be associated with EC risk and multivitamin and folic-acid supplementation may be associated with decreased EC risk. Early-adulthood overweight/obese weight-status and adulthood weight-gain may be associated with increased CRC risk, whereas multivitamin supplementation, tea and high fruit intake, and physical activity may be associated with decreased CRC risk. Current evidence proposes that recommendations related to weight, some dietary habits, and physical activity recommended for the general public are also relevant to individuals with lynch syndrome. More research is needed, specifically prospective cohorts and randomized controlled trials, to determine if tailored recommendations are needed among individuals with lynch syndrome.

Similar content being viewed by others
References
Spira A, Yurgelun M, Alexandrov L et al (2017) Precancer atlas to drive precision prevention trials. Cancer Res 77(7):1510–1541. https://doi.org/10.1158/0008-5472.CAN-16-2346
Aaltonen M, Staff S, Mecklin J, Pylvänäinen K, Mäenpää J (2017) Comparison of lifestyle, hormonal and medical factors in women with sporadic and Lynch syndrome-associated endometrial cancer: a retrospective case-case study. Mol Clin Oncol 6(5):758–764. https://doi.org/10.3892/mco.2017.1211
Aarnio M, Mecklin J, Aaltonen L, Nyström-Lahti M, Järvinen H (1995) Life-time risk of different cancers in hereditary non-polyposis colorectal cancer (HNPCC) syndrome. Int J Cancer 64(6):430–433
Lynch H, Lynch P, Lanspa S et al (2009) Review of the Lynch syndrome: history, molecular genetics, screening, differential diagnosis, and medicolegal ramifications. Clin Genet 76(1):1–18. https://doi.org/10.1111/j.1399-0004.2009.01230.x
Møller P, Seppälä T, Bernstein I et al (2017) Cancer risk and survival in path_MMR carriers by gene and gender up to 75 years of age: a report from the Prospective Lynch Syndrome Database. Gut. https://doi.org/10.1136/gutjnl-2017-314057
Møller P, Seppälä T, Bernstein I et al (2017) Cancer incidence and survival in Lynch syndrome patients receiving colonoscopic and gynaecological surveillance: first report from the prospective Lynch syndrome database. Gut 66(3):464–472. https://doi.org/10.1136/gutjnl-2015-309675
Diergaarde B, Braam H, Vasen H et al (2007) Environmental factors and colorectal tumor risk in individuals with hereditary nonpolyposis colorectal cancer. Clin Gastroenterol Hepatol 5(6):736–742
World Cancer Research Fund/American Institute for Cancer Research. Continuous update project expert report 2018. Diet, nutrition, physical activity and colorectal cancer. https://dietandcancerreport.org
World Cancer Research Fund/American Institute for Cancer Research. Continuous update project expert report 2018. Diet, nutrition, physical activity and endometrial cancer. https://dietandcancerreport.org
Filomeno M, Bosetti C, Bidoli E et al (2015) Mediterranean diet and risk of endometrial cancer: a pooled analysis of three Italian case-control studies. Br J Cancer 112(11):1816–1821. https://doi.org/10.1038/bjc.2015.153
Schwingshackl L, Hoffmann G (2016) Does a mediterranean-type diet reduce cancer risk? Curr Nutr Rep 5:9–17. https://doi.org/10.1007/s13668-015-0141-7
van Duijnhoven F, Botma A, Winkels R et al (2013) Do lifestyle factors influence colorectal cancer risk in Lynch syndrome? Fam Cancer 12(2):285–293. https://doi.org/10.1007/s10689-013-9645-8
Liberati A, Altman D, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1-34
Boyle T, Keegel T, Bull F, Heyworth J, Fritschi LP (2012) Activity and risks of proximal and distal colon cancers: a systematic review and meta-analysis. J Natl Cancer Inst 104(20):1548–1561. https://doi.org/10.1093/jnci/djs354
Singh S, Edakkanambeth Varayil J, Devanna S, Murad M, Iyer P (2014) Physical activity is associated with reduced risk of gastric cancer: a systematic review and meta-analysis. Cancer Prev Res (Phila) 7(1):12–22.
Maenpaa J, Aaltonen M, Mecklin J, Staff S (2016) Evaluation of factors modifying endometrial cancer risk among women with Lynch syndrome: a cohort study. J Clin Oncol 34:e17113
Win A, Chau R, Dashti S et al (2014) Lifestyle modifiers of risk of endometrial cancer for women with germline mutations in DNA mismatch repair genes. Int J Gynecol Cancer 24(9 suppl 4):1577–1578. https://doi.org/10.1097/01.IGC.0000457075.08973.89
Win A, Dowty J, Antill Y et al (2011) Body mass index in early adulthood and endometrial cancer risk for mismatch repair gene mutation carriers. Obstet Gynecol 117(4):899–905. https://doi.org/10.1097/AOG.0b013e3182110ea3
Botma A, Nagengast F, Braem M et al (2010) Body mass index increases risk of colorectal adenomas in men with Lynch syndrome: the GEOLynch cohort study. J Clin Oncol 28(28):4346–4353. https://doi.org/10.1200/JCO.2010.28.0453
Botma A, Vasen H, van Duijnhoven F et al (2013) Dietary patterns and colorectal adenomas in Lynch syndrome: the GEOLynch cohort study. Cancer 119(3):512–521. https://doi.org/10.1002/cncr.27726
Campbell P, Cotterchio M, Dicks E et al (2007) Excess body weight and colorectal cancer risk in Canada: associations in subgroups of clinically defined familial risk of cancer. Cancer Epidemiol Biomark Prev 16(9):1735–1744. https://doi.org/10.1158/1055-9965.EPI-06-1059
Chau R, Dashti S, Ait Ouakrim D et al (2016) Multivitamin, calcium and folic acid supplements and the risk of colorectal cancer in Lynch syndrome. Int J Epidemiol 45(3):940–953. https://doi.org/10.1093/ije/dyw036
Dashti S, Win W, Hardikar S et al (2018) Physical activity and the risk of colorectal cancer in Lynch Syndrome. Int J Cancer. https://doi.org/10.1002/ijc.31611 (Epub ahead of print)
Heine-Broring R, Winkels R, Botma A et al (2013) Dietary supplement use and colorectal adenoma risk in individuals with lynch syndrome: the GEOLynch Cohort Study. PLoS ONE 8(6):e66819. https://doi.org/10.1371/journal.pone.0066819
Kamiza A, Hsieh L, Tang R et al (2015) Risk Factors Associated with Colorectal Cancer in a Subset of Patients with Mutations in MLH1 and MSH2 in Taiwan Fulfilling the Amsterdam II Criteria for Lynch Syndrome. PLoS ONE 10(6):e0130018. https://doi.org/10.1371/journal.pone.0130018
Winkels R, Botma A, Nagengast F, Vasen H, Kampman E (2011) Smoking and alcohol consumption and colorectal adenoma risk in Lynch syndrome: the GEOLynch cohort study. Fam Cancer 10:S8. https://doi.org/10.1007/s10689-011-9424-3
Win A, Dowty J, English D et al (2011) Body mass index in early adulthood and colorectal cancer risk for carriers and non-carriers of germline mutations in DNA mismatch repair genes. Br J Cancer 105(1):162–169. https://doi.org/10.1038/bjc.2011.172
Dashti SG, Buchanan DD, Jayasekara H et al (2017) Alcohol consumption and the risk of colorectal cancer for mismatch repair gene mutation carriers. Cancer Epidemiol Biomark Prev 26(3):366–375. https://doi.org/10.1158/1055-9965.Epi-16-0496
Miguchi M, Hinoi T, Tanakaya K et al (2018) Alcohol consumption and early-onset risk of colorectal cancer in Japanese patients with Lynch syndrome: a cross-sectional study conducted by the Japanese Society for Cancer of the Colon and Rectum. Surg Today (Epub ahead of print). https://doi.org/10.1007/s00595-018-1654-7
Watson P, Ashwathnarayan R, Lynch HT, Roy HK (2004) Tobacco use and increased colorectal cancer risk in patients with hereditary nonpolyposis colorectal cancer (Lynch syndrome). Arch Intern Med 164:2429–2431
Winkels RM, Botma A, Van Duijnhoven FJ et al (2012) Smoking increases the risk for colorectal adenomas in patients with Lynch syndrome. Gastroenterology 142(2):241–247. https://doi.org/10.1053/j.gastro.2011.10.033
World Cancer Research Fund International/American Institute for Cancer Research (2013) Continuous update project report: food, nutrition, physical activity and the prevention of endometrial cancer. wcrf.org/sites/default/files/Endometrial-Cancer-2013-Report.pdf
Yoo H, Joo J, Seo S et al (2012) Correlation between body mass index and prevalence of hereditary nonpolyposis colorectal cancer in Korean patients with endometrial cancer. Int J Gynecol Cancer 22(2):267–272. https://doi.org/10.1097/IGC.0b013e31823b3650
Jain M, Rohan T, Howe G, Miller (2000) A A cohort study of nutritional factors and endometrial cancer. Eur J Epidemiol 16(10):899–905
Neuhouser M, Wassertheil-Smoller S, Thomson C et al (2009) Multivitamin use and risk of cancer and cardiovascular disease in the Women’s Health Initiative cohorts. Arch Intern Med 169(3):294–304. https://doi.org/10.1001/archinternmed.2008.540
Research WCRFIAIfC Continuous update project report: the association between food, nutrition, physical activity and the risk of endometrial cancer (2012)
Du L, Wang Y, Zhang H, Zhang H, Gao Y (2016) Folate intake and the risk of endometrial cancer: a meta-analysis. Oncotarget 7(51):85176–85184
McCann S, Freudenheim J, Marshall J et al (2000) Diet in the epidemiology of endometrial cancer in western New York (United States). Cancer Causes Control 11(10):965–974
Potischman N, Swanson C, Brinton L et al (1993) Dietary associations in a case-control study of endometrial cancer. Cancer Causes Control 4(3):239–250
Uccella S, Mariani A, Wang A et al (2011) Dietary and supplemental intake of one-carbon nutrients and the risk of type I and type II endometrial cancer: a prospective cohort study. Ann Oncol 22(9):2129–2136. https://doi.org/10.1093/annonc/mdq724
World Cancer Research Fund International/American Institute for Cancer Research (2017) Continuous update project report: diet, nutrition, physical activity and colorectal cancer. https://wcrf.org/colorectal-cancer-2017
Matsuo K, Mizoue T, Tanaka K et al (2012) Association between body mass index and the colorectal cancer risk in Japan: pooled analysis of population-based cohort studies in Japan. Ann Oncol 23(2):479–490. https://doi.org/10.1093/annonc/mdr143
Day D, Morson B (1978) The adenoma-carcinoma sequence. Major Probl Pathol 10:58–71
Hill M, Morson B, Bussey H (1978) Aetiology of adenoma–carcinoma sequence in large bowel. Lancet 1(8058):245–247
Okabayashi K, Ashrafian H, Hasegawa H et al (2012) Body mass index category as a risk factor for colorectal adenomas: a systematic review and meta-analysis. Am J Gastroenterol 107(8):1175–1185. https://doi.org/10.1038/ajg.2012.180
Aune D, Chan D, Vieira A et al (2013) Red and processed meat intake and risk of colorectal adenomas: a systematic review and meta-analysis of epidemiological studies. Cancer Causes Control 24(4):611–627. https://doi.org/10.1007/s10552-012-0139-z
Xu X, Yu E, Gao X et al (2013) Red and processed meat intake and risk of colorectal adenomas: a meta-analysis of observational studies. Int J Cancer 132(2):437–448. https://doi.org/10.1002/ijc.27625
Cottet V, Bonithon-Kopp C, Kronborg O et al (2005) Dietary patterns and the risk of colorectal adenoma recurrence in a European intervention trial. Eur J Cancer Prev 14(1):21–29
Lee I, Shiroma E, Lobelo F et al (2012) Effect of physical inactivity on major non-communicable disease worldwide: an analysis of burden of disease and life expectancy. Lancet 380:219–229
Schmid D, Leitzmann M (2014) Television viewing and time spent sedentary in relation to cancer risk: a meta-analysis. J Natl Cancer Inst. https://doi.org/10.1093/jnci/dju098
Giovannucci E, Ascherio A, Rimm E et al (1995) Physical activity, obesity, and risk for colon cancer and adenoma in men. Ann Intern Med 122:327–334
Acknowledgements
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number R25CA057730 (PI: Shine Chang, PhD), by the Center for Energy Balance in Cancer Prevention and Survivorship, Duncan Family Institute for Cancer Prevention and Risk Assessment, and by MRSG-13-145-01 from the American Cancer Society.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Coletta, A.M., Peterson, S.K., Gatus, L.A. et al. Energy balance related lifestyle factors and risk of endometrial and colorectal cancer among individuals with lynch syndrome: a systematic review. Familial Cancer 18, 399–420 (2019). https://doi.org/10.1007/s10689-019-00135-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-019-00135-7